Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
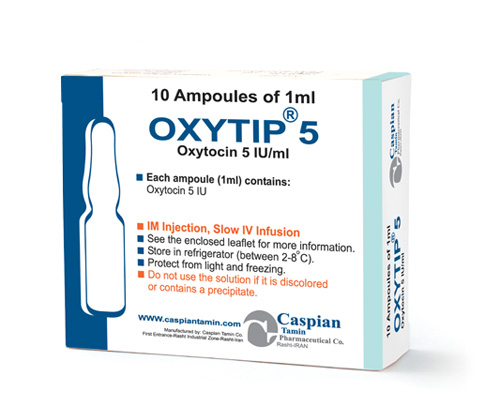
Oxytocin
Pharmacology
Oxytocin injection (synthetic) acts on the smooth muscle of the uterus to stimulate contractions; response depends on the uterine threshold of excitability. It exerts a selective action on the smooth musculature of the uterus, particularly toward the end of pregnancy, during labor and immediately following delivery. Oxytocin stimulates rhythmic contractions of the uterus, increases the frequency of existing contractions and raises the tone of the uterine musculature. Synthetic Oxytocin does not possess the cardiovascular effects, such as elevation of blood pressure, as exhibited by vasopressin found in posterior pituitary injection.
Pharmacokinetics:
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Indications:
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Contraindications:
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
Precautions:
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
Drug Interactions:
Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
Side Effects:
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
Storage:
• Store between 2-8C°
• Protect from light and freezing
Packing:
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
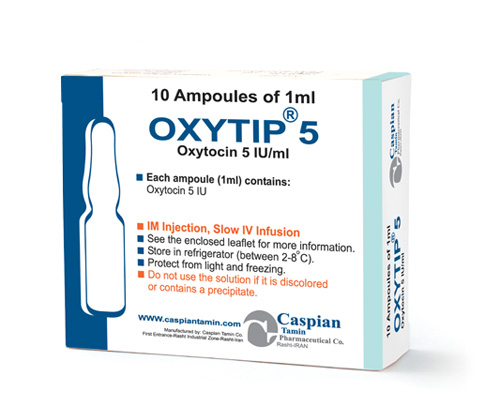
OXYTIP®
Injection 10U/1ml- Injection 5U/1ml
Pituitary Hormones
Oxytosics
Category X
Oxytocin injection (synthetic) acts on the smooth muscle of the uterus to stimulate contractions; response depends on the uterine threshold of excitability. It exerts a selective action on the smooth musculature of the uterus, particularly toward the end of pregnancy, during labor and immediately following delivery. Oxytocin stimulates rhythmic contractions of the uterus, increases the frequency of existing contractions and raises the tone of the uterine musculature. Synthetic Oxytocin does not possess the cardiovascular effects, such as elevation of blood pressure, as exhibited by vasopressin found in posterior pituitary injection.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
• Store between 2-8C°
• Protect from light and freezing
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => OXYTIP®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => OXYTIP®
[format] => 1
[safe] => OXYTIP®
[view] =>OXYTIP®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => • Significant cephalopelvic disproportion; • Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies; • In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention; • In cases of fetal distress where delivery is not imminent; • Prolonged use in uterine inertia or severe toxemia; • Hypertonic uterine patterns; • Patients with hypersensitivity to the drug; • Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa. [format] => 1 [safe] =>• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
Injection 10U/1ml- Injection 5U/1ml
[view] =>Injection 10U/1ml- Injection 5U/1ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia. [format] => 1 [safe] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
[view] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
) ) [field_indications] => Array ( [0] => Array ( [value] =>Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Pituitary Hormones
[view] =>Pituitary Hormones
) ) [field_precautions] => Array ( [0] => Array ( [value] => All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available. When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin. Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm. Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor. Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth. [format] => 1 [safe] =>All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
Category X
[view] =>Category X
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => The following adverse reactions have been reported in the mother: Anaphylactic reaction Nausea Postpartum hemorrhage Vomiting Cardiac arrhythmia Premature ventricular contractions Fatal afibrinogenemia Pelvic hematoma Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus. The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug. Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported. The following adverse reactions have been reported in the fetus or infant: Due to induced uterine mobility Due to use of Oxytocin in the mother Bradycardia Neonatal retinal hemorrhage Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes Permanent CNS or brain damage Neonatal jaundice Fetal death [format] => 1 [safe] =>The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
• Store between 2-8C°
• Protect from light and freezing
• Store between 2-8C°
• Protect from light and freezing
Oxytosics
[view] =>Oxytosics
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [5] => stdClass Object ( [tid] => 5 [vid] => 1 [name] => Hormonal Drugs [description] => [weight] => 3 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 235 [uid] => 1 [filename] => oxytocin_s.jpg [filepath] => sites/default/files/images/oxytocin_s.jpg [filemime] => image/jpeg [filesize] => 69348 [status] => 1 [timestamp] => 1329503915 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 265 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
OXYTIP®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>OXYTIP®
) [#title] => [#description] => [#children] =>OXYTIP®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>OXYTIP®
[#printed] => 1 ) [#title] => [#description] => [#children] =>OXYTIP®
Injection 10U/1ml- Injection 5U/1ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 10U/1ml- Injection 5U/1ml
) [#title] => [#description] => [#children] =>Injection 10U/1ml- Injection 5U/1ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 10U/1ml- Injection 5U/1ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 10U/1ml- Injection 5U/1ml
Pituitary Hormones
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Pituitary Hormones
) [#title] => [#description] => [#children] =>Pituitary Hormones
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Pituitary Hormones
[#printed] => 1 ) [#title] => [#description] => [#children] =>Pituitary Hormones
Oxytosics
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Oxytosics
) [#title] => [#description] => [#children] =>Oxytosics
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Oxytosics
[#printed] => 1 ) [#title] => [#description] => [#children] =>Oxytosics
Category X
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category X
) [#title] => [#description] => [#children] =>Category X
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category X
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category X
Oxytocin injection (synthetic) acts on the smooth muscle of the uterus to stimulate contractions; response depends on the uterine threshold of excitability. It exerts a selective action on the smooth musculature of the uterus, particularly toward the end of pregnancy, during labor and immediately following delivery. Oxytocin stimulates rhythmic contractions of the uterus, increases the frequency of existing contractions and raises the tone of the uterine musculature. Synthetic Oxytocin does not possess the cardiovascular effects, such as elevation of blood pressure, as exhibited by vasopressin found in posterior pituitary injection.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Absorption Onset IV administration: uterine response is almost immediate. IM injection: uterine response occurs within 3–5 minutes. IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes. Duration IV administration: uterine response subsides within 1 hour. IM injection: uterine response subsides in 2–3 hours. IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes. Plasma Concentrations IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor. Distribution Extent Distributed throughout the extracellular fluid. Crosses the placenta. Distributes into milk, probably in small amounts. Elimination Metabolism Rapidly metabolized in the liver and kidneys. Elimination Route Small amounts excreted in urine unchanged. [format] => 1 [safe] =>Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
) [#title] => [#description] => [#children] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_drug_interactions [#title] => Drug Interactions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
• Store between 2-8C°
• Protect from light and freezing
• Store between 2-8C°
• Protect from light and freezing
• Store between 2-8C°
• Protect from light and freezing
• Store between 2-8C°
• Protect from light and freezing
• Store between 2-8C°
• Protect from light and freezing
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules
OXYTIP®
Injection 10U/1ml- Injection 5U/1ml
Pituitary Hormones
Oxytosics
Category X
Oxytocin injection (synthetic) acts on the smooth muscle of the uterus to stimulate contractions; response depends on the uterine threshold of excitability. It exerts a selective action on the smooth musculature of the uterus, particularly toward the end of pregnancy, during labor and immediately following delivery. Oxytocin stimulates rhythmic contractions of the uterus, increases the frequency of existing contractions and raises the tone of the uterine musculature. Synthetic Oxytocin does not possess the cardiovascular effects, such as elevation of blood pressure, as exhibited by vasopressin found in posterior pituitary injection.
Absorption
Onset
IV administration: uterine response is almost immediate.
IM injection: uterine response occurs within 3–5 minutes.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts begin within a few minutes.
Duration
IV administration: uterine response subsides within 1 hour.
IM injection: uterine response subsides in 2–3 hours.
IV administration of 100–200 milliunits: contractions of myoepithelial tissue surrounding the alveoli of the breasts continue for 20 minutes.
Plasma Concentrations
IV infusion rates up to 6 milliunits/minute produce maternal oxytocin plasma concentrations comparable to those associated with spontaneous labor.
Distribution
Extent
Distributed throughout the extracellular fluid.
Crosses the placenta.
Distributes into milk, probably in small amounts.
Elimination
Metabolism
Rapidly metabolized in the liver and kidneys.
Elimination Route
Small amounts excreted in urine unchanged.
Antepartum
Oxytocin Injection, is indicated for the initiation or improvement of uterine contractions, where this is desirable and considered suitable, in order to achieve early vaginal delivery for fetal or maternal reasons. It is indicated for (1) induction of labor in patients with a medical indication for the initiation of labor, such as Rh problems, maternal diabetes, pre-eclampsia at or near term, when delivery is in the best interest of mother and fetus or when membranes are prematurely ruptured and delivery is indicated; (2) stimulation or reinforcement of labor, as in selected cases of uterine inertia; (3) adjunctive therapy in the management of incomplete or inevitable abortion. In the first trimester, curettage is generally considered primary therapy. In second trimester abortion, Oxytocin infusion will often be successful in emptying the uterus. Other means of therapy, however, may be required in such cases.
Postpartum
Oxytocin Injection, is indicated to produce uterine contractions during the third stage of labor and to control postpartum bleeding or hemorrhage.
• Significant cephalopelvic disproportion;
• Unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery, i.e., transverse lies;
• In obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention;
• In cases of fetal distress where delivery is not imminent;
• Prolonged use in uterine inertia or severe toxemia;
• Hypertonic uterine patterns;
• Patients with hypersensitivity to the drug;
• Induction or augmentation of labor in those cases where vaginal delivery is contraindicated, such as cord presentation or prolapse, total placenta previa, and vasa previa.
All patients receiving intravenous Oxytocin must be under continuous observation by trained personnel with a thorough knowledge of the drug and qualified to identify complications. A physician qualified to manage any complications should be immediately available.
When properly administered, Oxytocin should stimulate uterine contractions similar to those seen in normal labor. Overstimulation of the uterus by improper administration can be hazardous to both mother and fetus. Even with proper administration and adequate supervision, hypertonic contractions can occur in patients whose uteri are hypersensitive to Oxytocin.
Except in unusual circumstances, Oxytocin should not be administered in the following conditions: prematurity, borderline cephalopelvic disproportion, previous major surgery on the cervix or uterus including Caesarean section, overdistention of the uterus, grand multiparity or invasive cervical carcinoma. Because of the variability of the combinations of factors which may be present in the conditions above, the definition of “unusual circumstances” must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which Oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm.
Maternal deaths due to hypertensive episodes, subarachnoid hemorrhage, rupture of the uterus and fetal deaths due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor and for augmentation in the first and second stages of labor.
Oxytocin has been shown to have an intrinsic antidiuretic effect, acting to increase water reabsorption from the glomerular filtrate. Consideration should, therefore, be given to the possibility of water intoxication, particularly when Oxytocin is administered continuously by infusion and the patient is receiving fluids by mouth.
Severe hypertension has been reported when Oxytocin was given three to four hours following prophylactic administration of a vasoconstrictor in conjunction with caudal block anesthesia. Cyclopropane anesthesia may modify Oxytocin’s cardiovascular effects, so as to produce unexpected results such as hypotension. Maternal sinus bradycardia with abnormal atrioventricular rhythms has also been noted when Oxytocin was used concomitantly with cyclopropane anesthesia.
The following adverse reactions have been reported in the mother:
Anaphylactic reaction Nausea
Postpartum hemorrhage Vomiting
Cardiac arrhythmia Premature ventricular contractions
Fatal afibrinogenemia Pelvic hematoma
Excessive dosage or hypersensitivity to the drug may result in uterine hypertonicity, spasm, tetanic contraction or rupture of the uterus.
The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.
Severe water intoxication with convulsions and coma has occurred, and is associated with a slow Oxytocin infusion over a 24-hour period. Maternal death due to Oxytocin-induced water intoxication has been reported.
The following adverse reactions have been reported in the fetus or infant:
Due to induced uterine mobility Due to use of Oxytocin in the mother
Bradycardia Neonatal retinal hemorrhage
Premature ventricular contractions and other arrhythmias Low Apgar scores at five minutes
Permanent CNS or brain damage Neonatal jaundice
Fetal death
• Store between 2-8C°
• Protect from light and freezing
• Injection 10U/1ml: Box of 10,100Ampoules
• Injection 5U/1ml: Box of 10Ampoules