Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
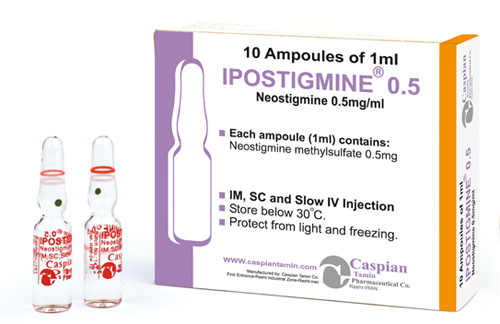
Neostigmine Methylsulfate
Pharmacology
Facilitates myoneural junction impulse transmission by inhibiting acetylcholine destruction by cholinesterase.
Pharmacokinetics:
Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
Indications:
Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
Contraindications:
Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
Precautions:
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
Drug Interactions:
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
Side Effects:
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Storage:
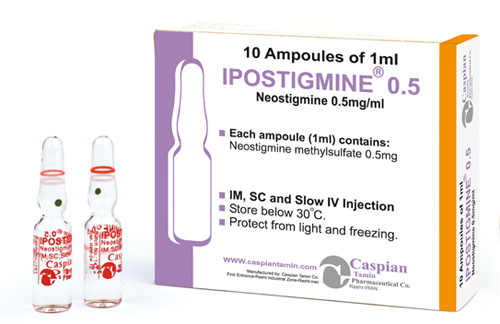
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
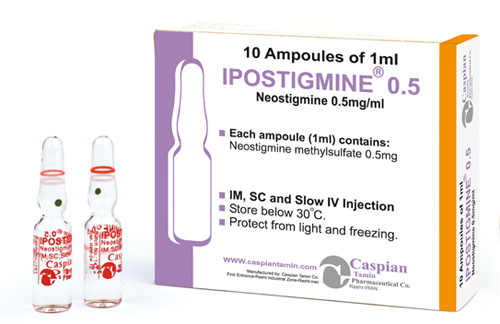
IPOSTIGMINE®
Injection 0.5mg/1ml - Injection2.5mg/1ml
Parasympathomimetic (Cholinergic) Agents
Antimyasthenic,Muscle Relaxant
category C
Facilitates myoneural junction impulse transmission by inhibiting acetylcholine destruction by cholinesterase.
Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
• Store below 30 C°
• Protect from light and freezing
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPOSTIGMINE®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPOSTIGMINE®
[format] => 1
[safe] => IPOSTIGMINE®
[view] =>IPOSTIGMINE®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis [format] => 1 [safe] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
[view] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 0.5mg/1ml - Injection2.5mg/1ml [format] => 1 [safe] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
[view] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => • Anticholinergic agents (eg, atropine, belladonna) Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed. • Beta-blockers (eg, propranolol) Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension. • Corticosteroids (eg, corticotropin, hydrocortisone) The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed. • Drugs that interfere with neuromuscular transmission May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed. • Kanamycin, streptomycin Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed. • Local/General anesthetics, antiarrhythmic agents (eg, procainamide) Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed. • Quinine Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis. • Succinylcholine Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed. [format] => 1 [safe] =>• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
[view] =>Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 0.5mg/1ml: Box of 10 Ampoules • Injection 2.5mg/1ml: Box of 10 Ampoules [format] => 1 [safe] =>• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
[view] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
) ) [field_pharmacological_category] => Array ( [0] => Array ( [value] => Parasympathomimetic (Cholinergic) Agents [format] => 1 [safe] =>Parasympathomimetic (Cholinergic) Agents
[view] =>Parasympathomimetic (Cholinergic) Agents
) ) [field_precautions] => Array ( [0] => Array ( [value] => • For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration. • Do not administer if particulate matter or discoloration is noted. • Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated. • Tablets • Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms. • Administer without regard to meals. Administer with food if GI upset occurs. • Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes). • Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract. • Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis. [format] => 1 [safe] =>• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
category C
[view] =>category C
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => Cardiovascular: Common (1% to 10%): Bradycardia, hypotension, tachycardia Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm) Dermatologic: Common (1% to 10%): Pruritus Frequency not reported: Rash, urticaria Gastrointestinal: Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting Frequency not reported: Flatulence, increased peristalsis Postmarketing reports: Bowel cramps, diarrhea Genitourinary: Frequency not reported: Urinary frequency Hypersensitivity: Frequency not reported: Allergic reactions and anaphylaxis Musculoskeletal: Frequency not reported: Muscle cramps and spasms, arthralgia Postmarketing reports: Muscle weakness Nervous system: Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness Ocular: Frequency not reported: Miosis, visual changes Other: Common (1% to 10%): Incision site complication, procedural complication and pain Frequency not reported: Diaphoresis, flushing, weakness Renal: Postmarketing reports: Urinary frequency Respiratory: Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%) Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm [format] => 1 [safe] =>Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Antimyasthenic,Muscle Relaxant
[view] =>Antimyasthenic,Muscle Relaxant
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [3] => stdClass Object ( [tid] => 3 [vid] => 1 [name] => Antimyasthenics ,Muscle Relaxants [description] => [weight] => 1 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 174 [uid] => 1 [filename] => neostigmine_s.jpg [filepath] => sites/default/files/images/neostigmine_s.jpg [filemime] => image/jpeg [filesize] => 67905 [status] => 1 [timestamp] => 1329487049 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 277 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
IPOSTIGMINE®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>IPOSTIGMINE®
) [#title] => [#description] => [#children] =>IPOSTIGMINE®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>IPOSTIGMINE®
[#printed] => 1 ) [#title] => [#description] => [#children] =>IPOSTIGMINE®
Injection 0.5mg/1ml - Injection2.5mg/1ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
) [#title] => [#description] => [#children] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 0.5mg/1ml - Injection2.5mg/1ml
Parasympathomimetic (Cholinergic) Agents
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Parasympathomimetic (Cholinergic) Agents
) [#title] => [#description] => [#children] =>Parasympathomimetic (Cholinergic) Agents
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Parasympathomimetic (Cholinergic) Agents
[#printed] => 1 ) [#title] => [#description] => [#children] =>Parasympathomimetic (Cholinergic) Agents
Antimyasthenic,Muscle Relaxant
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antimyasthenic,Muscle Relaxant
) [#title] => [#description] => [#children] =>Antimyasthenic,Muscle Relaxant
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antimyasthenic,Muscle Relaxant
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antimyasthenic,Muscle Relaxant
category C
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>category C
) [#title] => [#description] => [#children] =>category C
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>category C
[#printed] => 1 ) [#title] => [#description] => [#children] =>category C
Facilitates myoneural junction impulse transmission by inhibiting acetylcholine destruction by cholinesterase.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV). [format] => 1 [safe] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
) [#title] => [#description] => [#children] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacokinetics [#title] => Pharmacokinetics [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
[#printed] => 1 ) [#title] => [#description] => [#children] =>Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
) [#title] => [#description] => [#children] =>Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
[#printed] => 1 ) [#title] => [#description] => [#children] =>Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
) [#title] => [#description] => [#children] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
[#printed] => 1 ) [#title] => [#description] => [#children] =>Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules
IPOSTIGMINE®
Injection 0.5mg/1ml - Injection2.5mg/1ml
Parasympathomimetic (Cholinergic) Agents
Antimyasthenic,Muscle Relaxant
category C
Facilitates myoneural junction impulse transmission by inhibiting acetylcholine destruction by cholinesterase.
Rapid absorption, protein binding is 15% to 25% (serum albumin). Neostigmine is metabolized in the liver by microsomal enzymes and undergoes hydrolysis by cholinesterase. It`s is eliminated in urine (50% as unchanged). Half-life is 51 to 90 min and plasma half-life is 47 to 60 min (IV).
Symptomatic control of myasthenia gravis; antidote for nondepolarizing neuromuscular blocking agents after surgery; prevention and treatment of postoperative distention and urinary retention (IV only).
Hypersensitivity to anticholinesterases and bromides; mechanical intestinal or urinary obstruction; peritonitis
• For IV, subcutaneous, or IM administration. Not for intradermal or intra-arterial administration.
• Do not administer if particulate matter or discoloration is noted.
• Patients on IV neostigmine can be transferred to the oral form as soon as it can be tolerated.
• Tablets
• Administer as prescribed. Size of dose (eg, number of tablets) and frequency of administration will be adjusted to provide max relief of myasthenia gravis symptoms.
• Administer without regard to meals. Administer with food if GI upset occurs.
• Larger portions of the daily dose may be given at times when the patient is more prone to fatigue (eg, afternoons, mealtimes).
• Large doses should be avoided in situations where there might be an increased absorption rate from the intestinal tract.
• Ensure that parenteral atropine is available for emergency treatment of cholinergic crisis.
• Anticholinergic agents (eg, atropine, belladonna)
Intestinal motility may be slowed, increasing neostigmine absorption. Use with caution. Adjust the neostigmine dose as needed.
• Beta-blockers (eg, propranolol)
Severe or prolonged bradycardia may occur because of additive pharmacologic effects. Use with caution. Larger dosages of atropine and sympathomimetic pressor agents may be needed to reverse bradycardia and hypotension.
• Corticosteroids (eg, corticotropin, hydrocortisone)
The effects of neostigmine may be decreased. In addition, the effects of neostigmine may be increased after corticosteroids are discontinued. Provide mechanical respiratory support if needed.
• Drugs that interfere with neuromuscular transmission
May interfere with neuromuscular transmission. Use with caution in myasthenic patients. Monitor the patient and increase the neostigmine dose as needed.
• Kanamycin, streptomycin
Neuromuscular blockade may be enhanced. Use these antibiotics in myasthenic patients only when clearly indicated. Closely monitor the patient. Adjust the neostigmine dose as needed.
• Local/General anesthetics, antiarrhythmic agents (eg, procainamide)
Use with caution in myasthenic patients; may interfere with neuromuscular transmission. Increase the neostigmine dose as needed.
• Quinine
Quinine may antagonize the effects of neostigmine. Avoid using quinine in patients receiving neostigmine for myasthenia gravis.
• Succinylcholine
Neuromuscular blockade produced by succinylcholine may be prolonged. Avoid this combination in the presence of a depolarizing (phase 1) type of neuromuscular blockade. Use with caution if a nondepolarizing (phase 2) type of blockade is present. Provide mechanical respiratory support as needed.
Cardiovascular:
Common (1% to 10%): Bradycardia, hypotension, tachycardia
Frequency not reported: Nonspecific EKG changes, cardiac arrest, syncope
Postmarketing reports: Cardiac arrhythmias (A-V block, nodal rhythm)
Dermatologic:
Common (1% to 10%): Pruritus
Frequency not reported: Rash, urticaria
Gastrointestinal:
Common (1% to 10%): Dry mouth, nausea (including post-procedural), vomiting
Frequency not reported: Flatulence, increased peristalsis
Postmarketing reports: Bowel cramps, diarrhea
Genitourinary:
Frequency not reported: Urinary frequency
Hypersensitivity:
Frequency not reported: Allergic reactions and anaphylaxis
Musculoskeletal:
Frequency not reported: Muscle cramps and spasms, arthralgia
Postmarketing reports: Muscle weakness
Nervous system:
Common (1% to 10%): Dizziness, headache, postoperative shivering, prolonged neuromuscular blockade, insomnia
Postmarketing reports: Convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness
Ocular:
Frequency not reported: Miosis, visual changes
Other:
Common (1% to 10%): Incision site complication, procedural complication and pain
Frequency not reported: Diaphoresis, flushing, weakness
Renal:
Postmarketing reports: Urinary frequency
Respiratory:
Common (1% to 10%): Pharyngolaryngeal pain, dyspnea, oxygen desaturation (less than 90%)
Frequency not reported: Increased oral, pharyngeal and bronchial secretions, dyspnea, respiratory depression, respiratory arrest, bronchospasm
• Store below 30 C°
• Protect from light and freezing
• Injection 0.5mg/1ml: Box of 10 Ampoules
• Injection 2.5mg/1ml: Box of 10 Ampoules