Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Gentamicin
Pharmacology
After intramuscular administration of Gentamicin Sulfate, peak serum concentrations usually occur between 30 and 60 minutes and serum levels are measurable for 6 to 8 hours. In infants, a single dose of 2.5 mg/kg usually provides a peak serum level in the range of 3 to 5 mcg/mL. When gentamicin is administered by intravenous infusion over a two-hour period, the serum concentrations are similar to those obtained by intramuscular administration. Age markedly affects the peak concentrations: in one report, a 1 mg/kg dose produced mean peak concentrations of 1.58, 2.03, and 2.81 mcg/mL in patients six months to five years old, 5 to 10 years old, and over 10 years old, respectively.
In infants one week to six months of age, the half-life is 3 to 3 ½ hours. In full-term and large premature infants less than one week old, the approximate serum half-life of gentamicin is 5 ½ hours. In small premature infants, the half-life is inversely related to birth weight. In premature infants weighing less than 1500 grams, the half-life is 11 ½ hours; in those weighing 1500 to 2000 grams, the half-life is eight hours; in those weighing over 2000 grams, the half-life is approximately five hours. While some variation is to be expected due to a number of variables such as age, body temperature, surface area and physiologic differences, the individual patient given the same dose tends to have similar levels in repeated determinations.
Gentamicin, like all aminoglycosides, may accumulate in the serum and tissues of patients treated with higher doses and/or for prolonged periods, particularly in the presence of impaired or immature renal function. In patients with immature or impaired renal function, gentamicin is cleared from the body more slowly than in patients with normal renal function. The more severe the impairment, the slower the clearance. (Dosage must be adjusted.)
Since gentamicin is distributed in extracellular fluid, peak serum concentrations may be lower than usual in patients who have a large volume of this fluid. Serum concentrations of gentamicin in febrile patients may be lower than those in afebrile patients given the same dose. When body temperature returns to normal, serum concentrations of the drug may rise. Febrile and anemic states may be associated with a shorter than usual serum half-life. (Dosage adjustment is usually not necessary.) In severely burned patients, the half-life may be significantly decreased and resulting serum concentrations may be lower than anticipated from the mg/kg dose.
Protein-binding studies have indicated that the degree of gentamicin binding is low, depending upon the methods used for testing, this may be between 0 and 30%.
In neonates less than three days old, approximately 10% of the administered dose is excreted in 12 hours; in infants 5 to 40 days old, approximately 40% is excreted over the same period. Excretion of gentamicin correlates with postnatal age and creatinine clearance. Thus, with increasing postnatal age and concomitant increase in renal maturity, gentamicin is excreted more rapidly. Little, if any, metabolic transformation occurs; the drug is excreted principally by glomerular filtration. After several days of treatment, the amount of gentamicin excreted in the urine approaches, but does not equal, the daily dose administered. As with other aminoglycosides, a small amount of the gentamicin dose may be retained in the tissues, especially in the kidneys. Minute quantities of aminoglycosides have been detected in the urine of some patients weeks after drug administration was discontinued. Renal clearance of gentamicin is similar to that of endogenous creatinine.
In patients with marked impairment of renal function, there is a decrease in the concentration of aminoglycosides in urine and in their penetration into defective renal parenchyma. This decreased drug excretion, together with the potential nephrotoxicity of aminoglycosides, should be considered when treating such patients who have urinary tract infections.
Probenecid does not affect renal tubular transport of gentamicin.
The endogenous creatinine clearance rate and the serum creatinine level have a high correlation with the half-life of gentamicin in serum. Results of these tests may serve as guides for adjusting dosage in patients with renal impairment.
Following parenteral administration, gentamicin can be detected in serum, lymph, tissues, sputum, and in pleural, synovial, and peritoneal fluids. Concentrations in renal cortex sometimes may be eight times higher than the usual serum levels. Concentrations in bile, in general, have been low and have suggested minimal biliary excretion. Gentamicin crosses the peritoneal as well as the placental membranes. Since aminoglycosides diffuse poorly into the subarachnoid space after parenteral administration, concentrations of gentamicin in cerebrospinal fluid are often low and dependent upon dose, rate of penetration, and degree of meningeal inflammation. There is minimal penetration of gentamicin into ocular tissues following intramuscular or intravenous administration.
Pharmacokinetics:
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Indications:
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Contraindications:
Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
Precautions:
Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
Drug Interactions:
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Side Effects:
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
Storage:
• Store below 30 C°
• Protect from light and freezing
Packing:
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
GENTADIC®
Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
Aminoglycosides
Antibiotic
Category D
After intramuscular administration of Gentamicin Sulfate, peak serum concentrations usually occur between 30 and 60 minutes and serum levels are measurable for 6 to 8 hours. In infants, a single dose of 2.5 mg/kg usually provides a peak serum level in the range of 3 to 5 mcg/mL. When gentamicin is administered by intravenous infusion over a two-hour period, the serum concentrations are similar to those obtained by intramuscular administration. Age markedly affects the peak concentrations: in one report, a 1 mg/kg dose produced mean peak concentrations of 1.58, 2.03, and 2.81 mcg/mL in patients six months to five years old, 5 to 10 years old, and over 10 years old, respectively.
In infants one week to six months of age, the half-life is 3 to 3 ½ hours. In full-term and large premature infants less than one week old, the approximate serum half-life of gentamicin is 5 ½ hours. In small premature infants, the half-life is inversely related to birth weight. In premature infants weighing less than 1500 grams, the half-life is 11 ½ hours; in those weighing 1500 to 2000 grams, the half-life is eight hours; in those weighing over 2000 grams, the half-life is approximately five hours. While some variation is to be expected due to a number of variables such as age, body temperature, surface area and physiologic differences, the individual patient given the same dose tends to have similar levels in repeated determinations.
Gentamicin, like all aminoglycosides, may accumulate in the serum and tissues of patients treated with higher doses and/or for prolonged periods, particularly in the presence of impaired or immature renal function. In patients with immature or impaired renal function, gentamicin is cleared from the body more slowly than in patients with normal renal function. The more severe the impairment, the slower the clearance. (Dosage must be adjusted.)
Since gentamicin is distributed in extracellular fluid, peak serum concentrations may be lower than usual in patients who have a large volume of this fluid. Serum concentrations of gentamicin in febrile patients may be lower than those in afebrile patients given the same dose. When body temperature returns to normal, serum concentrations of the drug may rise. Febrile and anemic states may be associated with a shorter than usual serum half-life. (Dosage adjustment is usually not necessary.) In severely burned patients, the half-life may be significantly decreased and resulting serum concentrations may be lower than anticipated from the mg/kg dose.
Protein-binding studies have indicated that the degree of gentamicin binding is low, depending upon the methods used for testing, this may be between 0 and 30%.
In neonates less than three days old, approximately 10% of the administered dose is excreted in 12 hours; in infants 5 to 40 days old, approximately 40% is excreted over the same period. Excretion of gentamicin correlates with postnatal age and creatinine clearance. Thus, with increasing postnatal age and concomitant increase in renal maturity, gentamicin is excreted more rapidly. Little, if any, metabolic transformation occurs; the drug is excreted principally by glomerular filtration. After several days of treatment, the amount of gentamicin excreted in the urine approaches, but does not equal, the daily dose administered. As with other aminoglycosides, a small amount of the gentamicin dose may be retained in the tissues, especially in the kidneys. Minute quantities of aminoglycosides have been detected in the urine of some patients weeks after drug administration was discontinued. Renal clearance of gentamicin is similar to that of endogenous creatinine.
In patients with marked impairment of renal function, there is a decrease in the concentration of aminoglycosides in urine and in their penetration into defective renal parenchyma. This decreased drug excretion, together with the potential nephrotoxicity of aminoglycosides, should be considered when treating such patients who have urinary tract infections.
Probenecid does not affect renal tubular transport of gentamicin.
The endogenous creatinine clearance rate and the serum creatinine level have a high correlation with the half-life of gentamicin in serum. Results of these tests may serve as guides for adjusting dosage in patients with renal impairment.
Following parenteral administration, gentamicin can be detected in serum, lymph, tissues, sputum, and in pleural, synovial, and peritoneal fluids. Concentrations in renal cortex sometimes may be eight times higher than the usual serum levels. Concentrations in bile, in general, have been low and have suggested minimal biliary excretion. Gentamicin crosses the peritoneal as well as the placental membranes. Since aminoglycosides diffuse poorly into the subarachnoid space after parenteral administration, concentrations of gentamicin in cerebrospinal fluid are often low and dependent upon dose, rate of penetration, and degree of meningeal inflammation. There is minimal penetration of gentamicin into ocular tissues following intramuscular or intravenous administration.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
• Store below 30 C°
• Protect from light and freezing
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => GENTADIC®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => GENTADIC®
[format] => 1
[safe] => GENTADIC®
[view] =>GENTADIC®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class. [format] => 1 [safe] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
[view] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml [format] => 1 [safe] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
[view] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] =>Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Aminoglycosides
[view] =>Aminoglycosides
) ) [field_precautions] => Array ( [0] => Array ( [value] => Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins. Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it. Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy. A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections. Cross-allergenicity among aminoglycosides has been demonstrated. Patients should be well hydrated during treatment. Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin. Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated. Do not administer unless solution is clear and package undamaged. [format] => 1 [safe] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
[view] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
) ) [field_pregnancy_category] => Array ( [0] => Array ( [value] => Category D [format] => 1 [safe] =>Category D
[view] =>Category D
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] =>General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Antibiotic
[view] =>Antibiotic
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [10] => stdClass Object ( [tid] => 10 [vid] => 1 [name] => Antibacterials [description] => [weight] => 8 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 164 [uid] => 1 [filename] => 63_64_65_-gentadic_20-40-80_s.jpg [filepath] => sites/default/files/images/63_64_65_-gentadic_20-40-80_s.jpg [filemime] => image/jpeg [filesize] => 62186 [status] => 1 [timestamp] => 1329484778 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 246 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] => 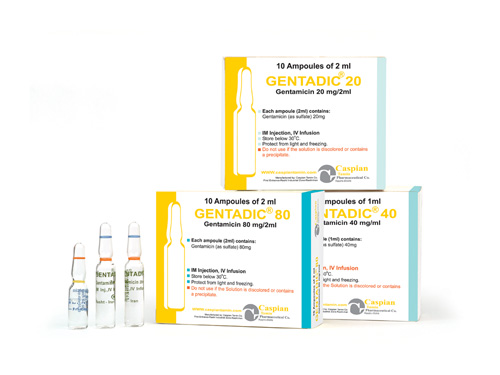 [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] => 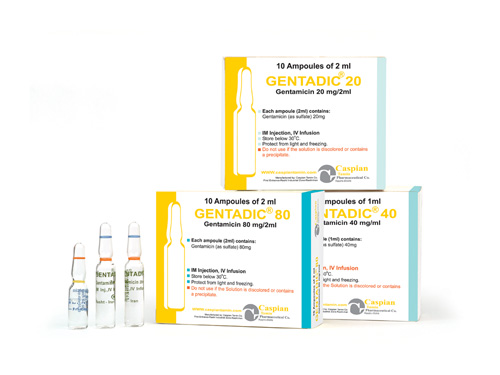 [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 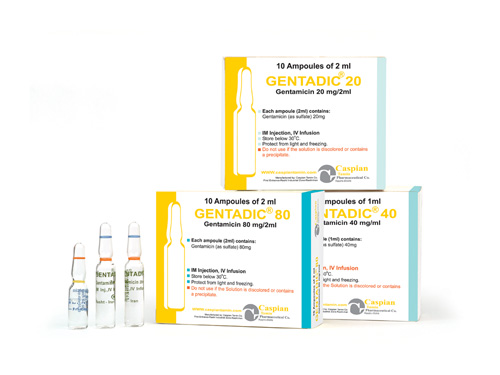
GENTADIC®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>GENTADIC®
) [#title] => [#description] => [#children] =>GENTADIC®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>GENTADIC®
[#printed] => 1 ) [#title] => [#description] => [#children] =>GENTADIC®
Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
) [#title] => [#description] => [#children] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
Aminoglycosides
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Aminoglycosides
) [#title] => [#description] => [#children] =>Aminoglycosides
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Aminoglycosides
[#printed] => 1 ) [#title] => [#description] => [#children] =>Aminoglycosides
Antibiotic
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antibiotic
) [#title] => [#description] => [#children] =>Antibiotic
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antibiotic
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antibiotic
Category D
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category D
) [#title] => [#description] => [#children] =>Category D
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category D
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category D
After intramuscular administration of Gentamicin Sulfate, peak serum concentrations usually occur between 30 and 60 minutes and serum levels are measurable for 6 to 8 hours. In infants, a single dose of 2.5 mg/kg usually provides a peak serum level in the range of 3 to 5 mcg/mL. When gentamicin is administered by intravenous infusion over a two-hour period, the serum concentrations are similar to those obtained by intramuscular administration. Age markedly affects the peak concentrations: in one report, a 1 mg/kg dose produced mean peak concentrations of 1.58, 2.03, and 2.81 mcg/mL in patients six months to five years old, 5 to 10 years old, and over 10 years old, respectively.
In infants one week to six months of age, the half-life is 3 to 3 ½ hours. In full-term and large premature infants less than one week old, the approximate serum half-life of gentamicin is 5 ½ hours. In small premature infants, the half-life is inversely related to birth weight. In premature infants weighing less than 1500 grams, the half-life is 11 ½ hours; in those weighing 1500 to 2000 grams, the half-life is eight hours; in those weighing over 2000 grams, the half-life is approximately five hours. While some variation is to be expected due to a number of variables such as age, body temperature, surface area and physiologic differences, the individual patient given the same dose tends to have similar levels in repeated determinations.
Gentamicin, like all aminoglycosides, may accumulate in the serum and tissues of patients treated with higher doses and/or for prolonged periods, particularly in the presence of impaired or immature renal function. In patients with immature or impaired renal function, gentamicin is cleared from the body more slowly than in patients with normal renal function. The more severe the impairment, the slower the clearance. (Dosage must be adjusted.)
Since gentamicin is distributed in extracellular fluid, peak serum concentrations may be lower than usual in patients who have a large volume of this fluid. Serum concentrations of gentamicin in febrile patients may be lower than those in afebrile patients given the same dose. When body temperature returns to normal, serum concentrations of the drug may rise. Febrile and anemic states may be associated with a shorter than usual serum half-life. (Dosage adjustment is usually not necessary.) In severely burned patients, the half-life may be significantly decreased and resulting serum concentrations may be lower than anticipated from the mg/kg dose.
Protein-binding studies have indicated that the degree of gentamicin binding is low, depending upon the methods used for testing, this may be between 0 and 30%.
In neonates less than three days old, approximately 10% of the administered dose is excreted in 12 hours; in infants 5 to 40 days old, approximately 40% is excreted over the same period. Excretion of gentamicin correlates with postnatal age and creatinine clearance. Thus, with increasing postnatal age and concomitant increase in renal maturity, gentamicin is excreted more rapidly. Little, if any, metabolic transformation occurs; the drug is excreted principally by glomerular filtration. After several days of treatment, the amount of gentamicin excreted in the urine approaches, but does not equal, the daily dose administered. As with other aminoglycosides, a small amount of the gentamicin dose may be retained in the tissues, especially in the kidneys. Minute quantities of aminoglycosides have been detected in the urine of some patients weeks after drug administration was discontinued. Renal clearance of gentamicin is similar to that of endogenous creatinine.
In patients with marked impairment of renal function, there is a decrease in the concentration of aminoglycosides in urine and in their penetration into defective renal parenchyma. This decreased drug excretion, together with the potential nephrotoxicity of aminoglycosides, should be considered when treating such patients who have urinary tract infections.
Probenecid does not affect renal tubular transport of gentamicin.
The endogenous creatinine clearance rate and the serum creatinine level have a high correlation with the half-life of gentamicin in serum. Results of these tests may serve as guides for adjusting dosage in patients with renal impairment.
Following parenteral administration, gentamicin can be detected in serum, lymph, tissues, sputum, and in pleural, synovial, and peritoneal fluids. Concentrations in renal cortex sometimes may be eight times higher than the usual serum levels. Concentrations in bile, in general, have been low and have suggested minimal biliary excretion. Gentamicin crosses the peritoneal as well as the placental membranes. Since aminoglycosides diffuse poorly into the subarachnoid space after parenteral administration, concentrations of gentamicin in cerebrospinal fluid are often low and dependent upon dose, rate of penetration, and degree of meningeal inflammation. There is minimal penetration of gentamicin into ocular tissues following intramuscular or intravenous administration.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
) [#title] => [#description] => [#children] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
) [#title] => [#description] => [#children] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_precautions [#title] => Precautions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)
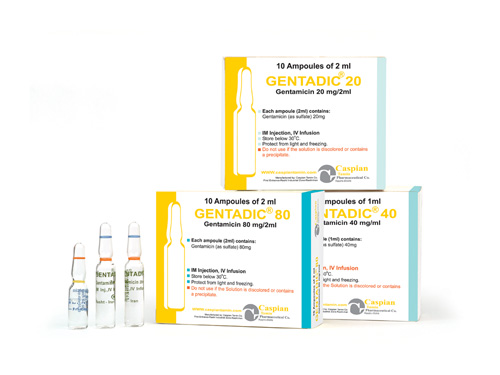
GENTADIC®
Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml
Aminoglycosides
Antibiotic
Category D
After intramuscular administration of Gentamicin Sulfate, peak serum concentrations usually occur between 30 and 60 minutes and serum levels are measurable for 6 to 8 hours. In infants, a single dose of 2.5 mg/kg usually provides a peak serum level in the range of 3 to 5 mcg/mL. When gentamicin is administered by intravenous infusion over a two-hour period, the serum concentrations are similar to those obtained by intramuscular administration. Age markedly affects the peak concentrations: in one report, a 1 mg/kg dose produced mean peak concentrations of 1.58, 2.03, and 2.81 mcg/mL in patients six months to five years old, 5 to 10 years old, and over 10 years old, respectively.
In infants one week to six months of age, the half-life is 3 to 3 ½ hours. In full-term and large premature infants less than one week old, the approximate serum half-life of gentamicin is 5 ½ hours. In small premature infants, the half-life is inversely related to birth weight. In premature infants weighing less than 1500 grams, the half-life is 11 ½ hours; in those weighing 1500 to 2000 grams, the half-life is eight hours; in those weighing over 2000 grams, the half-life is approximately five hours. While some variation is to be expected due to a number of variables such as age, body temperature, surface area and physiologic differences, the individual patient given the same dose tends to have similar levels in repeated determinations.
Gentamicin, like all aminoglycosides, may accumulate in the serum and tissues of patients treated with higher doses and/or for prolonged periods, particularly in the presence of impaired or immature renal function. In patients with immature or impaired renal function, gentamicin is cleared from the body more slowly than in patients with normal renal function. The more severe the impairment, the slower the clearance. (Dosage must be adjusted.)
Since gentamicin is distributed in extracellular fluid, peak serum concentrations may be lower than usual in patients who have a large volume of this fluid. Serum concentrations of gentamicin in febrile patients may be lower than those in afebrile patients given the same dose. When body temperature returns to normal, serum concentrations of the drug may rise. Febrile and anemic states may be associated with a shorter than usual serum half-life. (Dosage adjustment is usually not necessary.) In severely burned patients, the half-life may be significantly decreased and resulting serum concentrations may be lower than anticipated from the mg/kg dose.
Protein-binding studies have indicated that the degree of gentamicin binding is low, depending upon the methods used for testing, this may be between 0 and 30%.
In neonates less than three days old, approximately 10% of the administered dose is excreted in 12 hours; in infants 5 to 40 days old, approximately 40% is excreted over the same period. Excretion of gentamicin correlates with postnatal age and creatinine clearance. Thus, with increasing postnatal age and concomitant increase in renal maturity, gentamicin is excreted more rapidly. Little, if any, metabolic transformation occurs; the drug is excreted principally by glomerular filtration. After several days of treatment, the amount of gentamicin excreted in the urine approaches, but does not equal, the daily dose administered. As with other aminoglycosides, a small amount of the gentamicin dose may be retained in the tissues, especially in the kidneys. Minute quantities of aminoglycosides have been detected in the urine of some patients weeks after drug administration was discontinued. Renal clearance of gentamicin is similar to that of endogenous creatinine.
In patients with marked impairment of renal function, there is a decrease in the concentration of aminoglycosides in urine and in their penetration into defective renal parenchyma. This decreased drug excretion, together with the potential nephrotoxicity of aminoglycosides, should be considered when treating such patients who have urinary tract infections.
Probenecid does not affect renal tubular transport of gentamicin.
The endogenous creatinine clearance rate and the serum creatinine level have a high correlation with the half-life of gentamicin in serum. Results of these tests may serve as guides for adjusting dosage in patients with renal impairment.
Following parenteral administration, gentamicin can be detected in serum, lymph, tissues, sputum, and in pleural, synovial, and peritoneal fluids. Concentrations in renal cortex sometimes may be eight times higher than the usual serum levels. Concentrations in bile, in general, have been low and have suggested minimal biliary excretion. Gentamicin crosses the peritoneal as well as the placental membranes. Since aminoglycosides diffuse poorly into the subarachnoid space after parenteral administration, concentrations of gentamicin in cerebrospinal fluid are often low and dependent upon dose, rate of penetration, and degree of meningeal inflammation. There is minimal penetration of gentamicin into ocular tissues following intramuscular or intravenous administration.
Gentamicin is poorly absorbed after intramuscular injection. Average peak plasma concentrations of about 4 micrograms/mL have been attained in patients with normal renal function 30 to 60 minutes after an intramuscular dose equivalent to gentamicin 1 mg/kg, which is similar to concentrations achieved after intravenuos infusion. Several doses are required before plasma equilibrium concentrations occur and this may represent the saturation of binding sites in body tissues such as the kidney. Binding of gentamicin to plasma proteins is usually low.
On parenteral use, gentamicin and other aminoglycosides diffuse mainly into extracellular fluids.
However, there is little diffusion into the CSF and even when the meninges are inflamed effective concentrations may not be achieved; diffusion into the eye is also poor. Aminoglycosides diffuse readily into the perilymph of the inner ear. They cross the placenta but only small amounts have been reported in breast milk. Systemic absorption of gentamicin and other aminoglycosides has been reported.
Gentamicin Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter-Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown Gentamicin Injection to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, gentamicin may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin Injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgment indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of the known cross-sensitivity of patients to drugs in this class.
Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuromuscular blocking agents, such as succinylcholine, tubocurarine or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Aminoglycosides should be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs, and mental confusion have been described in patients with hypomagnesemia, hypocalcemia, and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with amino-aciduria and metabolic acidosis, has been reported in some adults and infants being given gentamicin injections.
Cross-allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
Do not administer unless solution is clear and package undamaged.
Major interactions:
Abobotulinumtoxina; amphotericin b; agalsidase alfa; atracurium; bacitracin; bcg vaccine live; bumetanide; cidofovir; cisatracurium; ethacrynic acid; furosemide; incobotulinumtoxina; neomycin; pancuronium; quinidine; rapacuronium; rocuronium; succinylcholine; torsemide; tubocurarine; typhoid vaccine live; vecuronium
Minor interactions:
Acyclovir; albuterol; amikacin; amiloride; amiodarone; aspirin; atenolol; betaxolol; bisoprolol; bumetanide; candesartan; carboplatin; carvedilol; celecoxib; chlorothiazide; cisplatin; clarithromycin; clotrimazole; conjugated estrogens; cyclosporine; deferasirox; diclofenac; estradiol valerate; digoxin; diltiazem; dobutamine; epinephrine; erythromycin; formoterol; furosemide; ibuprofen; indinavir; indomethacin(and other NSAIDs); irbesartan; isoproterenol; itraconazole; ketoconazole; loratadine; losartan; midazolam; phenobarbital; phenytoin; propranolol; salmeterol; rifampin; sirolimus; spironolactone; succinylcholine; sulfasalazine; tacrolimus; tenofovir; terbutaline; timolol; tolmetin; trazodone; triamterene; valsartan; verapamil
General
The most frequently reported adverse effects associated with gentamicin therapy are ototoxicity and nephrotoxicity. These forms of toxicity occur more frequently in patients who experience prolonged exposure to serum gentamicin trough concentrations of greater than 2 mcg/mL. Patients with renal insufficiency are at an increased risk of developing toxicity.
Renal
Renal side effects associated with gentamicin use have included nephrotoxicity. The overall incidence of aminoglycoside nephrotoxicity is 2% to 10%. Gentamicin nephrotoxicity occurs in two forms: acute renal failure (ARF), and a more gradual, transient, and reversible azotemia. Fanconi syndrome and Bartter-like syndrome have been reported.
Acute renal failure due to gentamicin is usually nonoliguric with an average rise in serum creatinine of 1 to 3 mg/dL. Renal function generally returns to baseline in 7 to 14 days. Rarely, gentamicin produces renal tubular acidosis and renal potassium and magnesium wasting. There is no relationship between acute renal failure and the daily dose of gentamicin, however, an increased incidence has been associated with a serum trough gentamicin concentration greater than 2 mcg/mL. It has been suggested that there is a correlation between the higher peak concentrations associated with once-daily dosing and a higher incidence of nephrotoxicity. Other predisposing factors include advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs.
Nervous system
The onset of ototoxicity may be asymptomatic or may manifest as dizziness, vertigo, ataxia, tinnitus, and roaring in the ears. High tone hearing loss is often an early symptom of auditory toxicity. It has been suggested that once-daily dosing of gentamicin is associated with a higher incidence of ototoxicity.
Other side effects possibly related to gentamicin have included lethargy, confusion, depression, headache, pseudotumor cerebri, and acute organic brain syndrome.
Nervous system side effects have included ototoxicity, which generally presents as loss of vestibular function secondary to hair cell damage, but may also be auditory. Ototoxicity is closely related to the development of renal impairment, and may be irreversible. Peripheral neuropathy or encephalopathy with numbness, skin tingling, muscle twitching, seizures, and myasthenia gravis-like syndrome have also been reported.
Intraventricular and intrathecal administration of gentamicin has rarely been associated with aseptic meningitis, transient hearing loss, and seizures. Neuromuscular side effects including ataxia, paresis and incontinence have been reported after large intrathecal doses (40 mg to 160 mg) of preservative-containing gentamicin. Concurrent administration of parenteral and intrathecal gentamicin has been associated with eighth nerve dysfunction, fever, convulsions, leg cramps, and increases in cerebrospinal fluid protein.
Musculoskeletal
Musculoskeletal side effects have rarely included neuromuscular blockade, which occurs most commonly in patients who are predisposed including patients with myasthenia gravis, hypocalcemia, and those receiving a concomitant neuromuscular blocking agent. Tetany and muscle weakness may be associated with gentamicin-induced hypomagnesemia, hypocalcemia, and hypokalemia. Joint pain has also been reported.
Respiratory
Respiratory side effects have included case reports of respiratory depression and respiratory arrest. Gentamicin has also been possibly associated with pulmonary fibrosis.
Hypersensitivity
Hypersensitivity reactions possibly associated with gentamicin have included anaphylactoid reactions and laryngeal edema. Suspected allergic reactions against gentamicin with sodium metabisulfite preservative have been reported.
Local
Local reactions have occasionally included pain at the injection site, and rarely subcutaneous atrophy or fat necrosis at the injection site. Reactions associated with intrathecal injections have included arachnoiditis and burning at the injection site.
Dermatologic
Dermatologic side effects possibly associated with gentamicin have included rash, itching, urticaria, generalized burning, and alopecia.
Hematologic
Hematologic side effects possibly related to gentamicin use have included anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts, thrombocytopenia, immunologic thrombocytopenia, and purpura.
Hepatic
Hepatic side effects possibly related to gentamicin use have included transient hepatomegaly, and increases in serum transaminase, serum LDH, and bilirubin.
Cardiovascular
Cardiovascular side effects possibly related to gentamicin have included hypotension and hypertension.
Gastrointestinal
Gastrointestinal side effects possibly related to gentamicin have included nausea, vomiting, weight loss, decreased appetite, increased salivation, and stomatitis.
Ocular
Ocular side effects have included case reports of retinal ischemia resulting in loss of visual acuity after inadvertent intraocular injection of massive doses of gentamicin.
Other
Other side effects possibly related to gentamicin have included transient splenomegaly and fever.
Pyrogenic reactions with symptoms of shaking, chills, fever, rigors, tachycardia, and/or hypotension have been reported with intravenous gentamicin. These reactions generally occurred within 3 hours of administration and were believed to be due to once-daily gentamicin doses delivering sufficient endotoxin over one hour to be pyrogenic.
• Store below 30 C°
• Protect from light and freezing
• Box of 10 ampoules (Injection 20mg/2ml, Injection 40mg/4ml, Injection 80mg/2ml)
• Box of 100 ampoules (Injection 80mg/2ml Ampoule)