Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
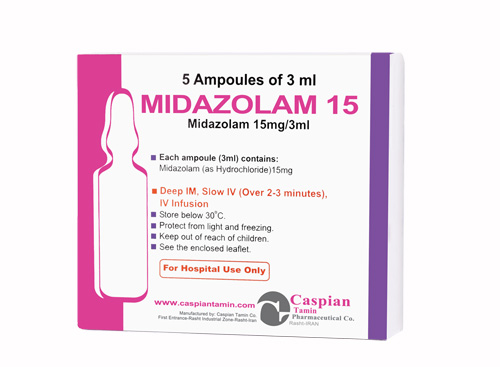
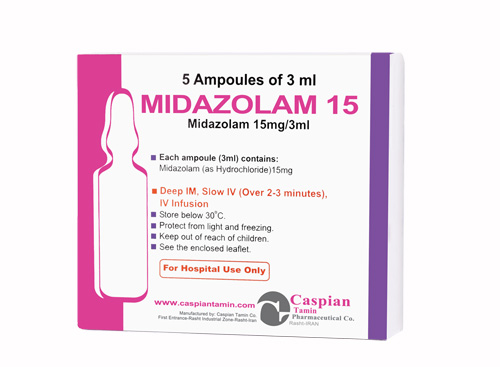
Midazolam
Pharmacology
Midazolam is a short-acting benzodiazepine central nervous system (CNS) depressant.The effects of midazolam on the CNS are dependent on the dose administered, the route of administration, and the presence or absence of other medications. Onset time of sedative effects after IM administration in adults is 15 minutes, with peak sedation occurring 30 to 60 minutes following injection.
Pharmacokinetics:
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Indications:
• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
Contraindications:
Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
Precautions:
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Drug Interactions:
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
Side Effects:
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
Storage:
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 15mg/3ml: Box of 5 Ampoules
-
Injection 15mg/3ml
Benzodiazepines
Sedative,hypnotic agent
Category D
Midazolam is a short-acting benzodiazepine central nervous system (CNS) depressant.The effects of midazolam on the CNS are dependent on the dose administered, the route of administration, and the presence or absence of other medications. Onset time of sedative effects after IM administration in adults is 15 minutes, with peak sedation occurring 30 to 60 minutes following injection.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• Store below 30 C°
• Protect from light and freezing
• Injection 15mg/3ml: Box of 5 Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => -
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => -
[format] => 1
[safe] => -
[view] =>-
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied. [format] => 1 [safe] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
[view] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 15mg/3ml [format] => 1 [safe] =>Injection 15mg/3ml
[view] =>Injection 15mg/3ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => • bosentan; • imatinib; • nefazodone; • St. John's wort; • an antibiotic--clarithromycin, erythromycin, telithromycin; • antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole; • heart medication--nicardipine, quinidine; • hepatitis C medications--boceprevir, telaprevir; • HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir; • seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or • tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine. [format] => 1 [safe] =>• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
[view] =>• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 15mg/3ml: Box of 5 Ampoules [format] => 1 [safe] =>• Injection 15mg/3ml: Box of 5 Ampoules
[view] =>• Injection 15mg/3ml: Box of 5 Ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 187 [uid] => 1 [filename] => midazolam.pdf [filepath] => sites/default/files/pdf/midazolam.pdf [filemime] => application/pdf [filesize] => 148625 [status] => 1 [timestamp] => 1329489464 [list] => 1 [data] => [i18nsync] => 1 [nid] => 271 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range. Absorption: The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr). Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection. Distribution: The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF. Metabolism: In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives. Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations. The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate. [format] => 1 [safe] =>Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Benzodiazepines
[view] =>Benzodiazepines
) ) [field_precautions] => Array ( [0] => Array ( [value] => Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia. Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia. [format] => 1 [safe] =>Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Category D
[view] =>Category D
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => • cough, wheezing, trouble breathing, weak or shallow breathing; • slow heart rate; • a light-headed feeling, like you might pass out; • agitation, hostility; or • confusion, hallucinations, unusual thoughts or behavior. Common side effects may include: • nausea, vomiting; • drowsiness, dizziness; • blurred vision; • runny nose, sneezing; or • amnesia or forgetfulness after your procedure. [format] => 1 [safe] =>• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Sedative,hypnotic agent
[view] =>Sedative,hypnotic agent
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [4] => stdClass Object ( [tid] => 4 [vid] => 1 [name] => Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics [description] => [weight] => 2 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 186 [uid] => 1 [filename] => midazolam_s.jpg [filepath] => sites/default/files/images/midazolam_s.jpg [filemime] => image/jpeg [filesize] => 60697 [status] => 1 [timestamp] => 1329489313 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 271 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
-
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>-
) [#title] => [#description] => [#children] =>-
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>-
[#printed] => 1 ) [#title] => [#description] => [#children] =>-
Injection 15mg/3ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 15mg/3ml
) [#title] => [#description] => [#children] =>Injection 15mg/3ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 15mg/3ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 15mg/3ml
Benzodiazepines
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Benzodiazepines
) [#title] => [#description] => [#children] =>Benzodiazepines
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Benzodiazepines
[#printed] => 1 ) [#title] => [#description] => [#children] =>Benzodiazepines
Sedative,hypnotic agent
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Sedative,hypnotic agent
) [#title] => [#description] => [#children] =>Sedative,hypnotic agent
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Sedative,hypnotic agent
[#printed] => 1 ) [#title] => [#description] => [#children] =>Sedative,hypnotic agent
Category D
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category D
) [#title] => [#description] => [#children] =>Category D
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category D
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category D
Midazolam is a short-acting benzodiazepine central nervous system (CNS) depressant.The effects of midazolam on the CNS are dependent on the dose administered, the route of administration, and the presence or absence of other medications. Onset time of sedative effects after IM administration in adults is 15 minutes, with peak sedation occurring 30 to 60 minutes following injection.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range. Absorption: The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr). Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection. Distribution: The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF. Metabolism: In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives. Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations. The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate. [format] => 1 [safe] =>Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
) [#title] => [#description] => [#children] =>• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
[#printed] => 1 ) [#title] => [#description] => [#children] =>• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
) [#title] => [#description] => [#children] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 15mg/3ml: Box of 5 Ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 15mg/3ml: Box of 5 Ampoules
) [#title] => [#description] => [#children] =>• Injection 15mg/3ml: Box of 5 Ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 15mg/3ml: Box of 5 Ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 15mg/3ml: Box of 5 Ampoules
-
Injection 15mg/3ml
Benzodiazepines
Sedative,hypnotic agent
Category D
Midazolam is a short-acting benzodiazepine central nervous system (CNS) depressant.The effects of midazolam on the CNS are dependent on the dose administered, the route of administration, and the presence or absence of other medications. Onset time of sedative effects after IM administration in adults is 15 minutes, with peak sedation occurring 30 to 60 minutes following injection.
Midazolam’s activity is primarily due to the parent drug. Elimination of the parent drug takes place via hepatic metabolism of midazolam to hydroxylated metabolites that are conjugated and excreted in the urine. Six single-dose pharmacokinetic studies involving healthy adults yield pharmacokinetic parameters for midazolam in the following ranges: volume of distribution (Vd), 1.0 to 3.1 L/kg; elimination half-life, 1.8 to 6.4 hours (mean approximately 3 hours); total clearance (Cl), 0.25 to 0.54 L/hr/kg. In a parallel group study, there was no difference in the clearance, in subjects administered 0.15 mg/kg (n=4) and 0.30 mg/kg (n=4) IV doses indicating linear kinetics. The clearance was successively reduced by approximately 30% at doses of 0.45 mg/kg (n=4) and 0.6 mg/kg (n=5) indicating non-linear kinetics in this dose range.
Absorption:
The absolute bioavailability of the intramuscular route was greater than 90% in a cross-over study in which healthy subjects (n=17) were administered a 7.5 mg IV or IM dose. The mean peak concentration (Cmax) and time to peak (Tmax) following the IM dose was 90 ng/mL (20% CV) and 0.5 hr (50% CV). Cmax for the 1-hydroxy metabolite following the IM dose was 8 ng/mL (Tmax =1.0 hr).
Following IM administration, Cmax for midazolam and its 1-hydroxy metabolite were approximately one-half of those achieved after intravenous injection.
Distribution:
The volume of distribution (Vd) determined from six single-dose pharmacokinetic studies involving healthy adults ranged from 1.0 to 3.1 L/kg. Female gender, old age, and obesity are associated with increased values of midazolam Vd. In humans, midazolam has been shown to cross the placenta and enter into fetal circulation and has been detected in human milk and CSF.
Metabolism:
In vitro studies with human liver microsomes indicate that the biotransformation of midazolam is mediated by cytochrome P450 3A4. This cytochrome also appears to be present in gastrointestinal tract mucosa as well as liver. Sixty to seventy percent of the biotransformation products is 1-hydroxymidazolam (also termed alpha-hydroxymidazolam) while 4-hydroxy- midazolam constitutes 5% or less. Small amounts of a dihydroxy derivative have also been detected but not quantified. The principal urinary excretion products are glucuronide conjugates of the hydroxylated derivatives.
Drugs that inhibit the activity of the cytochrome P450 3A4 may inhibit midazolam clearance and elevate steady-state midazolam concentrations.
The principal urinary excretion product is 1-hydroxy-midazolam in the form of a glucuronide conjugate; smaller amounts of the glucuronide conjugates of 4-hydroxy- and dihydroxy- midazolam are detected as well. The amount of midazolam excreted unchanged in the urine after a single IV dose is less than 0.5% (n=5). Following a single IV infusion in 5 healthy volunteers, 45% to 57% of the dose was excreted in the urine as 1-hydroxymethyl midazolam conjugate.
• intravenously as an agent for sedation/anxiolysis/amnesia prior to or during diagnostic, therapeutic or endoscopic procedures, such as bronchoscopy, gastroscopy, cystoscopy, coronary angiography, cardiac catheterization, oncology procedures, radiologic procedures, suture of lacerations and other procedures either alone or in combination with other CNS depressants;
• intravenously for induction of general anesthesia, before administration of other anesthetic agents. With the use of narcotic premedication, induction of anesthesia can be attained within a relatively narrow dose range and in a short period of time. Intravenous midazolam can also be used as a component of intravenous supplementation of nitrous oxide and oxygen (balanced anesthesia);
Injectable midazolam hydrochloride is contraindicated in patients with a known hypersensitivity to the drug. Benzodiazepines are contraindicated in patients with acute narrow-angle glaucoma. Benzodiazepines may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. Measurements of intraocular pressure in patients without eye disease show a moderate lowering following induction with midazolam hydrochloride; patients with glaucoma have not been studied.
Intravenous doses of midazolam hydrochloride should be decreased for elderly and for debilitated patients. These patients will also probably take longer to recover completely after midazolam administration for the induction of anesthesia.
Midazolam does not protect against the increase in intracranial pressure or against the heart rate rise and/or blood pressure rise associated with endotracheal intubation under light general anesthesia.
• bosentan;
• imatinib;
• nefazodone;
• St. John's wort;
• an antibiotic--clarithromycin, erythromycin, telithromycin;
• antifungal medication--itraconazole, ketoconazole, posaconazole, voriconazole;
• heart medication--nicardipine, quinidine;
• hepatitis C medications--boceprevir, telaprevir;
• HIV/AIDS medication--atazanavir, delavirdine, efavirenz, fosamprenavir, indinavir, nelfinavir, nevirapine, ritonavir, saquinavir;
• seizure medication--carbamazepine, fosphenytoin, oxcarbazepine, phenobarbital, phenytoin, primidone; or
• tuberculosis medication--isoniazid, rifabutin, rifampin, rifapentine.
• cough, wheezing, trouble breathing, weak or shallow breathing;
• slow heart rate;
• a light-headed feeling, like you might pass out;
• agitation, hostility; or
• confusion, hallucinations, unusual thoughts or behavior.
Common side effects may include:
• nausea, vomiting;
• drowsiness, dizziness;
• blurred vision;
• runny nose, sneezing; or
• amnesia or forgetfulness after your procedure.
• Store below 30 C°
• Protect from light and freezing
• Injection 15mg/3ml: Box of 5 Ampoules