Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Lidocaine
Pharmacology
Studies of the effects of therapeutic concentrations of Lidocaine on the electrophysiological properties of mammalian Purkinje fibers have shown that Lidocaine attenuates phase 4 diastolic depolarization, decreases automaticity and causes a decrease or no change in excitability and membrane responsiveness. Action potential duration and effective refractory period of Purkinje fibers are decreased while the ratio of effective refractory period to action potential duration is increased. Action potential duration and effective refractory period of ventricular muscle are also decreased. Effective refractory period of the AV node may increase, decrease or remain unchanged and atrial effective refractory period is unchanged. Lidocaine raises the ventricular fibrillation threshold. No significant interactions between Lidocaine and the autonomic nervous system have been described and consequently Lidocaine has little or no effect on autonomic tone.
Clinical electrophysiological studies with Lidocaine have demonstrated no change in sinus node recovery time or sinoatrial conduction time. AV nodal conduction time is unchanged or shortened and His-Purkinje conduction time is unchanged.
At therapeutic doses, Lidocaine has minimal hemodynamic effects in normal subjects and in patients with heart disease. Lidocaine has been shown to cause no, or minimal decrease in ventricular contractility, cardiac output, arterial pressure or heart rate.
Pharmacokinetics:
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Indications:
Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
Contraindications:
Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
Precautions:
Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
Drug Interactions:
Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
Side Effects:
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Storage:
• Store below 30 C°
• Protect from light and freezing
Packing:
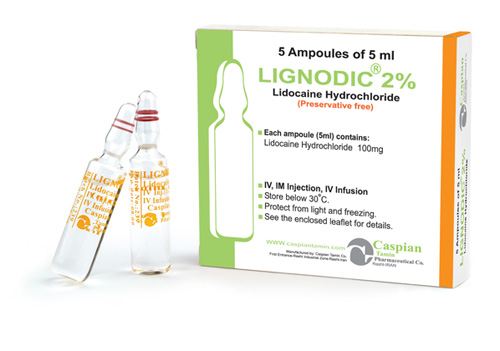
• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
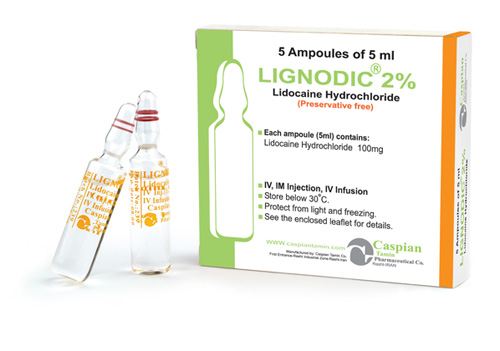
LIGNODIC ®
Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
Antiarrhythmic
General/Local Anaesthetics
Category B
Studies of the effects of therapeutic concentrations of Lidocaine on the electrophysiological properties of mammalian Purkinje fibers have shown that Lidocaine attenuates phase 4 diastolic depolarization, decreases automaticity and causes a decrease or no change in excitability and membrane responsiveness. Action potential duration and effective refractory period of Purkinje fibers are decreased while the ratio of effective refractory period to action potential duration is increased. Action potential duration and effective refractory period of ventricular muscle are also decreased. Effective refractory period of the AV node may increase, decrease or remain unchanged and atrial effective refractory period is unchanged. Lidocaine raises the ventricular fibrillation threshold. No significant interactions between Lidocaine and the autonomic nervous system have been described and consequently Lidocaine has little or no effect on autonomic tone.
Clinical electrophysiological studies with Lidocaine have demonstrated no change in sinus node recovery time or sinoatrial conduction time. AV nodal conduction time is unchanged or shortened and His-Purkinje conduction time is unchanged.
At therapeutic doses, Lidocaine has minimal hemodynamic effects in normal subjects and in patients with heart disease. Lidocaine has been shown to cause no, or minimal decrease in ventricular contractility, cardiac output, arterial pressure or heart rate.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
• Store below 30 C°
• Protect from light and freezing
• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => LIGNODIC ®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => LIGNODIC ®
[format] => 1
[safe] => LIGNODIC ®
[view] =>LIGNODIC ®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker. [format] => 1 [safe] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
[view] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%) [format] => 1 [safe] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
[view] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure. [format] => 1 [safe] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
[view] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
) ) [field_indications] => Array ( [0] => Array ( [value] => Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery. [format] => 1 [safe] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
[view] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml ) [format] => 1 [safe] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
[view] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 226 [uid] => 1 [filename] => lidocaine.pdf [filepath] => sites/default/files/pdf/lidocaine.pdf [filemime] => application/pdf [filesize] => 593748 [status] => 1 [timestamp] => 1329496465 [list] => 1 [data] => [i18nsync] => 1 [nid] => 245 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline. The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours. Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites. Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL. The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein. Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine. [format] => 1 [safe] =>Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Antiarrhythmic
[view] =>Antiarrhythmic
) ) [field_precautions] => Array ( [0] => Array ( [value] => Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur. Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block. Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status. The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients. In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available. It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene. [format] => 1 [safe] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
[view] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
) ) [field_pregnancy_category] => Array ( [0] => Array ( [value] => Category B [format] => 1 [safe] =>Category B
[view] =>Category B
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe. 1. Central Nervous System: CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest. 2. Cardiovascular System: Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest. 3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means. 4. Neurologic: There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration. [format] => 1 [safe] =>Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
General/Local Anaesthetics
[view] =>General/Local Anaesthetics
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [9] => stdClass Object ( [tid] => 9 [vid] => 1 [name] => General Anaesthetics, Local Anaesthetics [description] => [weight] => 7 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 225 [uid] => 1 [filename] => lidocaine_s.jpg [filepath] => sites/default/files/images/lidocaine_s.jpg [filemime] => image/jpeg [filesize] => 64345 [status] => 1 [timestamp] => 1329496209 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 245 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>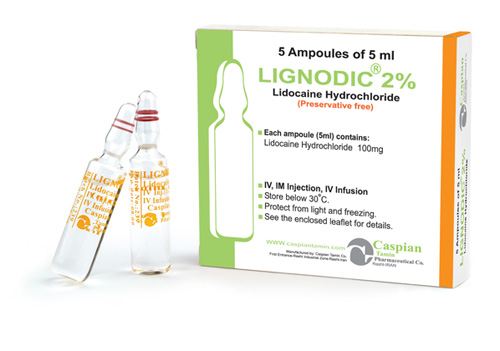 )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] => 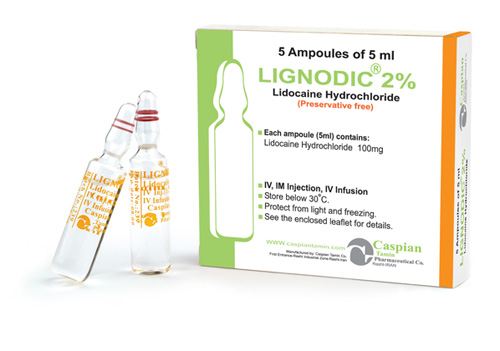 [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] => 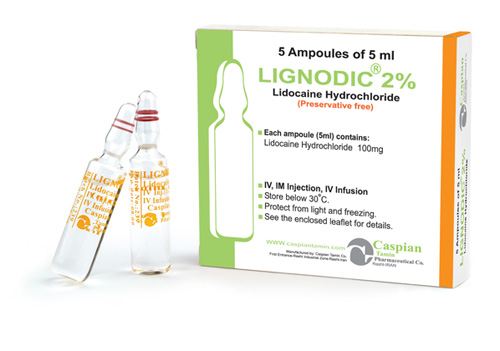 [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 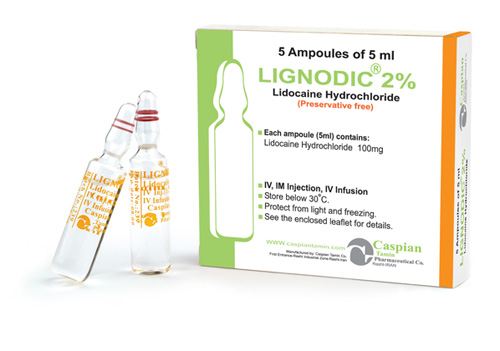
LIGNODIC ®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>LIGNODIC ®
) [#title] => [#description] => [#children] =>LIGNODIC ®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>LIGNODIC ®
[#printed] => 1 ) [#title] => [#description] => [#children] =>LIGNODIC ®
Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
) [#title] => [#description] => [#children] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
Antiarrhythmic
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antiarrhythmic
) [#title] => [#description] => [#children] =>Antiarrhythmic
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antiarrhythmic
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antiarrhythmic
General/Local Anaesthetics
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>General/Local Anaesthetics
) [#title] => [#description] => [#children] =>General/Local Anaesthetics
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>General/Local Anaesthetics
[#printed] => 1 ) [#title] => [#description] => [#children] =>General/Local Anaesthetics
Category B
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category B
) [#title] => [#description] => [#children] =>Category B
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category B
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category B
Studies of the effects of therapeutic concentrations of Lidocaine on the electrophysiological properties of mammalian Purkinje fibers have shown that Lidocaine attenuates phase 4 diastolic depolarization, decreases automaticity and causes a decrease or no change in excitability and membrane responsiveness. Action potential duration and effective refractory period of Purkinje fibers are decreased while the ratio of effective refractory period to action potential duration is increased. Action potential duration and effective refractory period of ventricular muscle are also decreased. Effective refractory period of the AV node may increase, decrease or remain unchanged and atrial effective refractory period is unchanged. Lidocaine raises the ventricular fibrillation threshold. No significant interactions between Lidocaine and the autonomic nervous system have been described and consequently Lidocaine has little or no effect on autonomic tone.
Clinical electrophysiological studies with Lidocaine have demonstrated no change in sinus node recovery time or sinoatrial conduction time. AV nodal conduction time is unchanged or shortened and His-Purkinje conduction time is unchanged.
At therapeutic doses, Lidocaine has minimal hemodynamic effects in normal subjects and in patients with heart disease. Lidocaine has been shown to cause no, or minimal decrease in ventricular contractility, cardiac output, arterial pressure or heart rate.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
) [#title] => [#description] => [#children] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
) [#title] => [#description] => [#children] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
) [#title] => [#description] => [#children] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_precautions [#title] => Precautions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
) [#title] => [#description] => [#children] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_drug_interactions [#title] => Drug Interactions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
) [#title] => [#description] => [#children] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )
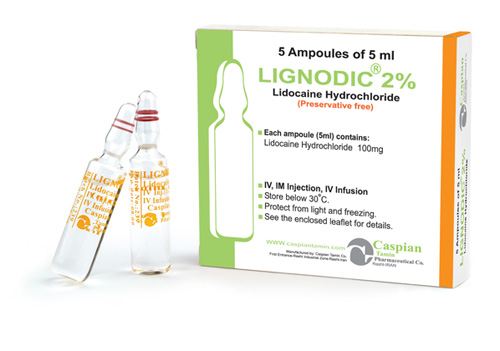
LIGNODIC ®
Injection 50mg/5m (1%), 100mg/5ml (2%), Spinal (lidocaine hydrochloride 5% + Dextrose 7.5%)
Antiarrhythmic
General/Local Anaesthetics
Category B
Studies of the effects of therapeutic concentrations of Lidocaine on the electrophysiological properties of mammalian Purkinje fibers have shown that Lidocaine attenuates phase 4 diastolic depolarization, decreases automaticity and causes a decrease or no change in excitability and membrane responsiveness. Action potential duration and effective refractory period of Purkinje fibers are decreased while the ratio of effective refractory period to action potential duration is increased. Action potential duration and effective refractory period of ventricular muscle are also decreased. Effective refractory period of the AV node may increase, decrease or remain unchanged and atrial effective refractory period is unchanged. Lidocaine raises the ventricular fibrillation threshold. No significant interactions between Lidocaine and the autonomic nervous system have been described and consequently Lidocaine has little or no effect on autonomic tone.
Clinical electrophysiological studies with Lidocaine have demonstrated no change in sinus node recovery time or sinoatrial conduction time. AV nodal conduction time is unchanged or shortened and His-Purkinje conduction time is unchanged.
At therapeutic doses, Lidocaine has minimal hemodynamic effects in normal subjects and in patients with heart disease. Lidocaine has been shown to cause no, or minimal decrease in ventricular contractility, cardiac output, arterial pressure or heart rate.
Lidocaine is rapidly metabolized by the liver and less than 10% of a dose is excreted unchanged in the urine. Oxidative N-dealkylation, a major pathway of metabolism, results in the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological activities of these metabolites are similar to but less potent than Lidocaine. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline.
The elimination half-life of Lidocaine following an intravenous bolus injection is typically 1.5 to 2 hours. There are data that indicate that the half-life may be 3 hours or longer following infusions of greater than 24 hours.
Because of the rapid rate at which Lidocaine is metabolized, any condition that alters liver function, including changes in liver blood flow, which could result from severe congestive heart failure or shock may alter Lidocaine kinetics. The half-life may be two-fold or more greater in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine kinetics, but may increase the accumulation of metabolites.
Therapeutic effects of Lidocaine are generally associated with plasma levels of 6 to 25 μmole/L (1.5 to 6 mcg free base per mL). The blood to plasma distribution ratio is approximately 0.84. Objective adverse manifestations become increasingly apparent with increasing plasma levels above 6 mcg free base per mL.
The plasma protein binding of Lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg free base per mL, 60 to 80 percent of Lidocaine is protein bound. In addition to Lidocaine concentration, the binding is dependent on the plasma concentration of the α-1-acid glycoprotein.
Lidocaine readily crosses the placental and blood-brain barriers. Dialysis has negligible effects on the kinetics of Lidocaine.
Lidocaine hydrochloride injection administered intravenously or intramuscularly, is specifically indicated in the acute management of ventricular arrhythmias such as those occurring in relation to acute myocardial infarction, or during cardiac manipulation, such as cardiac surgery.
Lidocaine hydrochloride is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type. Lidocaine hydrochloride should not be used in patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome or with severe degrees of sinoatrial, atrioventricular or intraventricular block in the absence of an artificial pacemaker.
Aution should be employed in the use of Lidocaine hydrochloride in patients with severe liver or kidney disease because accumulation of the drug or metabolites may occur.
Lidocaine Hydrochloride should be used with caution in the treatment of patients with hypovolemia, severe congestive heart failure, shock and all forms of heart block. In patients with sinus bradycardia or incomplete heart block, the administration of Lidocaine hydrochloride intravenously for the elimination of ventricular ectopic beats without prior acceleration in heart rate (e.g., by atropine, isoproterenol or electric pacing) may promote more frequent and serious ventricular arrhythmias or complete heart block.
Dosage should be reduced for pediatric patients and for debilitated and/or elderly patients, commensurate with their age and physical status.
The safety of amide local anesthetic agents in patients with genetic predisposition of malignant hyperthermia has not been fully assessed; therefore, Lidocaine should be used with caution in such patients.
In hospital environments where drugs known to be triggering agents for malignant hyperthermia (fulminant hypermetabolism) are administered, it is suggested that a standard protocol for management should be available.
It is not known whether Lidocaine may trigger this reaction; however, large doses resulting in significant plasma concentrations, as may be achieved by intravenous infusion, pose potential risk to these individuals. Recognition of early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the triggering agent and institution of treatment including oxygen therapy, supportive measures and dantrolene.
Lidocaine Hydrochloride should be used with caution in patients with digitalis toxicity accompanied by atrioventricular block. Concomitant use of beta-blocking agents or cimetidine may reduce hepatic blood flow and thereby reduce Lidocaine clearance. The concomitant use of these two agents may cause an increased incidence of adverse reactions, including central nervous system adverse reactions such as seizure.
Adverse experiences following the administration of Lidocaine are similar in nature to those observed with other amide local anesthetic agents. Adverse experiences may result from high plasma levels caused by excessive dosage or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported. The adverse experiences under Central Nervous System and Cardiovascular System are listed, in general, in a progression from mild to severe.
1. Central Nervous System:
CNS reactions are excitatory and/or depressant and may be characterized by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory reactions may be very brief or may not occur at all, in which case, the first manifestation of toxicity may be drowsiness, merging into unconsciousness and respiratory arrest.
2. Cardiovascular System:
Cardiovascular reactions are usually depressant in nature and are characterized by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
3. Allergic reactions as a result of sensitivity to Lidocaine are extremely rare and, if they occur, should be managed by conventional means.
4. Neurologic:
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
• Store below 30 C°
• Protect from light and freezing
• Injection 50mg/5m (1%), 100mg/5ml (2%):Box of 5 ampoules (Injection 50mg/5m, 100mg/5ml )