Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
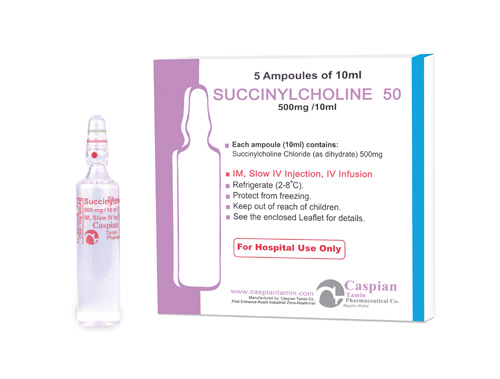
Succinyl Choline
Pharmacology
Succinylcholine is a depolarizing skeletal muscle relaxant. As does acetylcholine, it combines with the cholinergic receptors of the motor end plate to produce depolarization. This depolarization may be observed as fasciculations. Subsequent neuromuscular transmission is inhibited so long as adequate concentration of succinylcholine remains at the receptor site. Onset of flaccid paralysis is rapid (less than 1 minute after IV administration), and with single administration lasts approximately 4 to 6 minutes.
Pharmacokinetics:
Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
Indications:
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
Contraindications:
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Precautions:
Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
Drug Interactions:
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Side Effects:
Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
Storage:
• Store between 2-8 C°
• Protect from light and freezing
Packing:
• Injection 500mg/10ml:Box of 5 Ampoules
-
Injection 500mg/10ml
Neuromuscular Blocking Agents
Antimyasthenic, Muscle Relaxant
category C
Succinylcholine is a depolarizing skeletal muscle relaxant. As does acetylcholine, it combines with the cholinergic receptors of the motor end plate to produce depolarization. This depolarization may be observed as fasciculations. Subsequent neuromuscular transmission is inhibited so long as adequate concentration of succinylcholine remains at the receptor site. Onset of flaccid paralysis is rapid (less than 1 minute after IV administration), and with single administration lasts approximately 4 to 6 minutes.
Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
• Store between 2-8 C°
• Protect from light and freezing
• Injection 500mg/10ml:Box of 5 Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => -
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => -
[format] => 1
[safe] => -
[view] =>-
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Personal or familial history of malignant hyperthermia. • Myopathies associated with elevated serum creatine kinase (CK, CPK) values. • Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.) • Known hypersensitivity to succinylcholine or any ingredient in the formulation. [format] => 1 [safe] =>Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Injection 500mg/10ml
[view] =>Injection 500mg/10ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] =>|
β-Adrenergic blocking agents |
Possible increased neuromuscular blockade |
|
|
Anesthetics, inhalation (e.g., desflurane, isoflurane) |
Possible increased neuromuscular blockade |
|
|
Antiarrhythmic agents (lidocaine, procainamide, quinidine) |
Possible increased neuromuscular blockade |
|
|
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines) |
Possible increased neuromuscular blockade |
|
|
Antimalarials (chloroquine, quinine) |
Possible increased neuromuscular blockade |
|
|
Aprotinin |
Possible increased neuromuscular blockade |
|
|
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides) |
Decreased activity of plasma pseudocholinesterase |
|
|
Contraceptives, oral |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Corticosteroids |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Cyclophosphamide |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Lithium |
Possible increased neuromuscular blockade |
|
|
Magnesium salts |
Possible increased neuromuscular blockade |
|
|
MAO inhibitors |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Metoclopramide |
Possible increased neuromuscular blockade |
|
|
Neostigmine |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Oxytocin |
Possible increased neuromuscular blocking effect |
|
|
Phenothiazines |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Procaine |
Potential decreased metabolism of succinylcholine |
Concurrent IV administration not recommended |
|
Skeletal muscle relaxants (pancuronium) |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Terbutaline |
Possible increased neuromuscular blockade |
|
|
Thiotepa |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
[format] => 1 [safe] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
[view] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
) ) [field_indications] => Array ( [0] => Array ( [value] => • Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia. • Drug of choice for skeletal muscle relaxation during orthopedic manipulations. • Treatment to increase pulmonary compliance during assisted or controlled respiration. [format] => 1 [safe] =>
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Injection 500mg/10ml:Box of 5 Ampoules
[view] =>• Injection 500mg/10ml:Box of 5 Ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 179 [uid] => 1 [filename] => succinylcholine.pdf [filepath] => sites/default/files/pdf/succinylcholine.pdf [filemime] => application/pdf [filesize] => 135676 [status] => 1 [timestamp] => 1329487795 [list] => 1 [data] => [i18nsync] => 1 [nid] => 275 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg. Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes. The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds. [format] => 1 [safe] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
[view] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
) ) [field_pharmacological_category] => Array ( [0] => Array ( [value] => Neuromuscular Blocking Agents [format] => 1 [safe] =>Neuromuscular Blocking Agents
[view] =>Neuromuscular Blocking Agents
) ) [field_precautions] => Array ( [0] => Array ( [value] => Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma. Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect. Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents. Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia. Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents. [format] => 1 [safe] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
[view] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
) ) [field_pregnancy_category] => Array ( [0] => Array ( [value] => category C [format] => 1 [safe] =>category C
[view] =>category C
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles. [format] => 1 [safe] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
[view] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
) ) [field_storage] => Array ( [0] => Array ( [value] => • Store between 2-8 C° • Protect from light and freezing [format] => 1 [safe] =>• Store between 2-8 C°
• Protect from light and freezing
• Store between 2-8 C°
• Protect from light and freezing
Antimyasthenic, Muscle Relaxant
[view] =>Antimyasthenic, Muscle Relaxant
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [3] => stdClass Object ( [tid] => 3 [vid] => 1 [name] => Antimyasthenics ,Muscle Relaxants [description] => [weight] => 1 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 178 [uid] => 1 [filename] => succinylcholine_s.jpg [filepath] => sites/default/files/images/succinylcholine_s.jpg [filemime] => image/jpeg [filesize] => 55226 [status] => 1 [timestamp] => 1329487646 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 275 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
-
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>-
) [#title] => [#description] => [#children] =>-
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>-
[#printed] => 1 ) [#title] => [#description] => [#children] =>-
Injection 500mg/10ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 500mg/10ml
) [#title] => [#description] => [#children] =>Injection 500mg/10ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 500mg/10ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 500mg/10ml
Neuromuscular Blocking Agents
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Neuromuscular Blocking Agents
) [#title] => [#description] => [#children] =>Neuromuscular Blocking Agents
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Neuromuscular Blocking Agents
[#printed] => 1 ) [#title] => [#description] => [#children] =>Neuromuscular Blocking Agents
Antimyasthenic, Muscle Relaxant
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antimyasthenic, Muscle Relaxant
) [#title] => [#description] => [#children] =>Antimyasthenic, Muscle Relaxant
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antimyasthenic, Muscle Relaxant
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antimyasthenic, Muscle Relaxant
category C
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>category C
) [#title] => [#description] => [#children] =>category C
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>category C
[#printed] => 1 ) [#title] => [#description] => [#children] =>category C
Succinylcholine is a depolarizing skeletal muscle relaxant. As does acetylcholine, it combines with the cholinergic receptors of the motor end plate to produce depolarization. This depolarization may be observed as fasciculations. Subsequent neuromuscular transmission is inhibited so long as adequate concentration of succinylcholine remains at the receptor site. Onset of flaccid paralysis is rapid (less than 1 minute after IV administration), and with single administration lasts approximately 4 to 6 minutes.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg. Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes. The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds. [format] => 1 [safe] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
) [#title] => [#description] => [#children] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacokinetics [#title] => Pharmacokinetics [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
) [#title] => [#description] => [#children] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_precautions [#title] => Precautions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
|
β-Adrenergic blocking agents |
Possible increased neuromuscular blockade |
|
|
Anesthetics, inhalation (e.g., desflurane, isoflurane) |
Possible increased neuromuscular blockade |
|
|
Antiarrhythmic agents (lidocaine, procainamide, quinidine) |
Possible increased neuromuscular blockade |
|
|
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines) |
Possible increased neuromuscular blockade |
|
|
Antimalarials (chloroquine, quinine) |
Possible increased neuromuscular blockade |
|
|
Aprotinin |
Possible increased neuromuscular blockade |
|
|
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides) |
Decreased activity of plasma pseudocholinesterase |
|
|
Contraceptives, oral |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Corticosteroids |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Cyclophosphamide |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Lithium |
Possible increased neuromuscular blockade |
|
|
Magnesium salts |
Possible increased neuromuscular blockade |
|
|
MAO inhibitors |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Metoclopramide |
Possible increased neuromuscular blockade |
|
|
Neostigmine |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Oxytocin |
Possible increased neuromuscular blocking effect |
|
|
Phenothiazines |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Procaine |
Potential decreased metabolism of succinylcholine |
Concurrent IV administration not recommended |
|
Skeletal muscle relaxants (pancuronium) |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
|
|
Terbutaline |
Possible increased neuromuscular blockade |
|
|
Thiotepa |
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade |
[format] => 1 [safe] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
) [#title] => [#description] => [#children] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_drug_interactions [#title] => Drug Interactions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
[#printed] => 1 ) [#title] => [#description] => [#children] =>
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
) [#title] => [#description] => [#children] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_side_effects [#title] => Side Effects [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
• Store between 2-8 C°
• Protect from light and freezing
• Store between 2-8 C°
• Protect from light and freezing
• Store between 2-8 C°
• Protect from light and freezing
• Store between 2-8 C°
• Protect from light and freezing
• Store between 2-8 C°
• Protect from light and freezing
• Injection 500mg/10ml:Box of 5 Ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 500mg/10ml:Box of 5 Ampoules
) [#title] => [#description] => [#children] =>• Injection 500mg/10ml:Box of 5 Ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 500mg/10ml:Box of 5 Ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 500mg/10ml:Box of 5 Ampoules
-
Injection 500mg/10ml
Neuromuscular Blocking Agents
Antimyasthenic, Muscle Relaxant
category C
Succinylcholine is a depolarizing skeletal muscle relaxant. As does acetylcholine, it combines with the cholinergic receptors of the motor end plate to produce depolarization. This depolarization may be observed as fasciculations. Subsequent neuromuscular transmission is inhibited so long as adequate concentration of succinylcholine remains at the receptor site. Onset of flaccid paralysis is rapid (less than 1 minute after IV administration), and with single administration lasts approximately 4 to 6 minutes.
Succinylcholine is the only available neuromuscular blocker with a rapid onset of effect and an ultrashort duration of action. The ED95 of succinylcholine (the dose causing on average 95% suppression of neuromuscular response) is 0.51 to 0.63 mg/kg. Using cumulative dose-response techniques, Kopman and coworkers estimated that its potency is far greater, with an ED95 of less than 0.3 mg/kg.
Administration of 1 mg/kg of succinylcholine results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds. In patients with genotypically normal butyrylcholinesterase (also known as plasma cholinesterase or pseudocholinesterase) activity, recovery to 90% muscle strength after the administration of 1 mg/kg succinylcholine requires 9 to 13 minutes.
The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase to succinylmonocholine and choline. Butyrylcholinesterase has an enormous capacity to hydrolyze succinylcholine, and only 10% of the administered drug reaches the neuromuscular junction. The initial metabolite, succinylmonocholine, is a much weaker neuromuscular blocking agent than succinylcholine and is metabolized much more slowly to succinic acid and choline. The elimination half-life of succinylcholine is estimated to be 47 seconds.
• Production of skeletal muscle relaxation during procedures of short duration (e.g., endotracheal intubation, endoscopic examinations, electrically or pharmacologically induced convulsive therapy) after general anesthesia.
• Drug of choice for skeletal muscle relaxation during orthopedic manipulations.
• Treatment to increase pulmonary compliance during assisted or controlled respiration.
Personal or familial history of malignant hyperthermia.
• Myopathies associated with elevated serum creatine kinase (CK, CPK) values.
• Upper motor neuron injury, multiple trauma, extensive or severe burns, extensive denervation of skeletal muscle because of CNS disease or injury. (See Hyperkalemia under Cautions.)
• Known hypersensitivity to succinylcholine or any ingredient in the formulation.
Succinylcholine should be employed with caution in patients with fractures or muscle spasm because the initial muscle fasciculations may cause additional trauma.
Succinylcholine may cause a transient increase in intracranial pressure; however, adequate anesthetic induction prior to administration of succinylcholine will minimize this effect.
Succinylcholine may increase intragastric pressure, which could result in regurgitation and possible aspiration of stomach contents.
Neuromuscular blockade may be prolonged in patients with hypokalemia or hypocalcemia.
Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents.
β-Adrenergic blocking agents
Possible increased neuromuscular blockade
Anesthetics, inhalation (e.g., desflurane, isoflurane)
Possible increased neuromuscular blockade
Antiarrhythmic agents (lidocaine, procainamide, quinidine)
Possible increased neuromuscular blockade
Anti-infective agents (aminoglycosides, bacitracin, clindamycin, lincomycin, polymyxins, tetracyclines)
Possible increased neuromuscular blockade
Antimalarials (chloroquine, quinine)
Possible increased neuromuscular blockade
Aprotinin
Possible increased neuromuscular blockade
Cholinesterase inhibitors (demecarium, isofluorophate, organophosphate insecticides)
Decreased activity of plasma pseudocholinesterase
Contraceptives, oral
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Corticosteroids
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Cyclophosphamide
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Lithium
Possible increased neuromuscular blockade
Magnesium salts
Possible increased neuromuscular blockade
MAO inhibitors
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Metoclopramide
Possible increased neuromuscular blockade
Neostigmine
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Oxytocin
Possible increased neuromuscular blocking effect
Phenothiazines
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Procaine
Potential decreased metabolism of succinylcholine
Concurrent IV administration not recommended
Skeletal muscle relaxants (pancuronium)
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Terbutaline
Possible increased neuromuscular blockade
Thiotepa
Possible decreased plasma cholinesterase activity and increased neuromuscular blockade
Severe allergic reactions (rash; hives; itching; difficulty breathing; tightness in the chest; swelling of the mouth, face, lips, or tongue); chest pain; fainting; fast breathing; fast, slow, or irregular heartbeat; flushing; high body temperature; increased pressure in the eye; pauses in breathing; pounding in the chest; severe muscle pain with or without decreased urination; severe or persistent dizziness or headache; slowed or shallow breathing; tightening of the jaw or other muscles.
• Store between 2-8 C°
• Protect from light and freezing
• Injection 500mg/10ml:Box of 5 Ampoules