Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
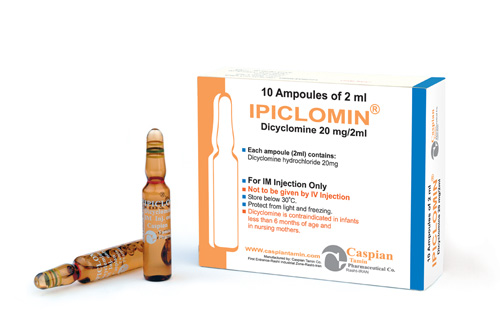
Dicyclomine
Pharmacology
Dicyclomine relieves smooth muscle spasm of the gastrointestinal tract. Animal studies indicate that this action is achieved via a dual mechanism: (1) a specific anticholinergic effect (antimuscarinic) at the acetylcholine-receptor sites with approximately 1/8 the milligram potency of atropine (in vitro, guinea pig ileum); and (2) a direct effect upon smooth muscle (musculotropic) as evidenced by Dicyclomine’s antagonism of bradykinin- and histamine-induced spasms of the isolated guinea pig ileum. Atropine did not affect responses to these two agonists. In vivo studies in cats and dogs showed Dicyclomine to be equally potent against acetylcholine (ACh)- or barium chloride (BaCl2)-induced intestinal spasm while atropine was at least 200 times more potent against effects of ACh than BaCl2. Tests for mydriatic effects in mice showed that Dicyclomine was approximately 1/500 as potent as atropine; antisialagogue tests in rabbits showed Dicyclomine to be 1/300 as potent as atropine.
Dicyclomine can inhibit the secretion of saliva and sweat, decrease gastrointestinal secretions and motility, cause drowsiness, dilate the pupils, increase heart rate, and depress motor function.
Pharmacokinetics:
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Indications:
Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
Contraindications:
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
Precautions:
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Drug Interactions:
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
Side Effects:
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Storage:
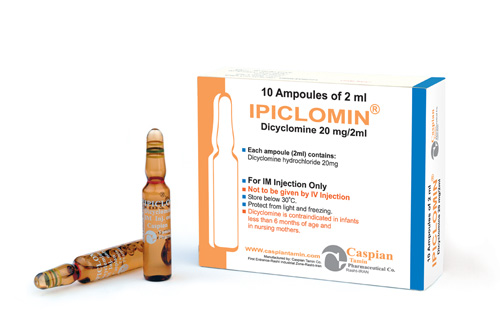
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 20mg/2ml: Box of 10 ampoules
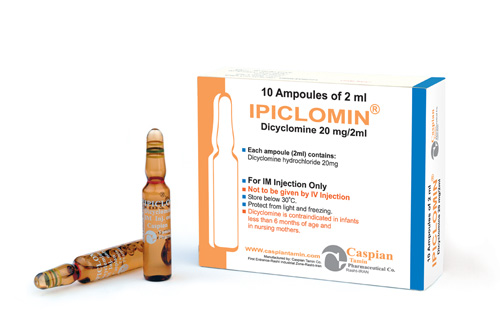
IPICLOMIN®
Injection 20mg/2ml
Antispasmodic/Anticholinegic
Gastrointestinal drugs
Category B
Dicyclomine relieves smooth muscle spasm of the gastrointestinal tract. Animal studies indicate that this action is achieved via a dual mechanism: (1) a specific anticholinergic effect (antimuscarinic) at the acetylcholine-receptor sites with approximately 1/8 the milligram potency of atropine (in vitro, guinea pig ileum); and (2) a direct effect upon smooth muscle (musculotropic) as evidenced by Dicyclomine’s antagonism of bradykinin- and histamine-induced spasms of the isolated guinea pig ileum. Atropine did not affect responses to these two agonists. In vivo studies in cats and dogs showed Dicyclomine to be equally potent against acetylcholine (ACh)- or barium chloride (BaCl2)-induced intestinal spasm while atropine was at least 200 times more potent against effects of ACh than BaCl2. Tests for mydriatic effects in mice showed that Dicyclomine was approximately 1/500 as potent as atropine; antisialagogue tests in rabbits showed Dicyclomine to be 1/300 as potent as atropine.
Dicyclomine can inhibit the secretion of saliva and sweat, decrease gastrointestinal secretions and motility, cause drowsiness, dilate the pupils, increase heart rate, and depress motor function.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
• Store below 30 C°
• Protect from light and freezing
• Injection 20mg/2ml: Box of 10 ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPICLOMIN®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPICLOMIN®
[format] => 1
[safe] => IPICLOMIN®
[view] =>IPICLOMIN®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => • Obstructive uropathy • Obstructive disease of the gastrointestinal tract • Severe ulcerative colitis • Reflux esophagitis • Unstable cardiovascular status in acute hemorrhage • Glaucoma • Myasthenia gravis • Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation • Infants less than 6 months of age • Nursing Mothers [format] => 1 [safe] =>• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
Injection 20mg/2ml
[view] =>Injection 20mg/2ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity. Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids. Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided. The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion. [format] => 1 [safe] =>The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
[view] =>Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 20mg/2ml: Box of 10 ampoules [format] => 1 [safe] =>• Injection 20mg/2ml: Box of 10 ampoules
[view] =>• Injection 20mg/2ml: Box of 10 ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 216 [uid] => 1 [filename] => dicyclomine.pdf [filepath] => sites/default/files/pdf/dicyclomine.pdf [filemime] => application/pdf [filesize] => 145565 [status] => 1 [timestamp] => 1329495276 [list] => 1 [data] => [i18nsync] => 1 [nid] => 253 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] =>Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Antispasmodic/Anticholinegic
[view] =>Antispasmodic/Anticholinegic
) ) [field_precautions] => Array ( [0] => Array ( [value] => Use with caution in patients with: • Autonomic neuropathy • Hepatic or renal disease • Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon • Hyperthyroidism • Hypertension • Coronary heart disease • Congestive heart failure • Cardiac tachyarrhythmia • Hiatal hernia • Known or suspected prostatic hypertrophy. Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate. With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis). [format] => 1 [safe] =>Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Category B
[view] =>Category B
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] =>Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Gastrointestinal drugs
[view] =>Gastrointestinal drugs
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [11] => stdClass Object ( [tid] => 11 [vid] => 1 [name] => Gastrointestinal Drugs [description] => [weight] => 9 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 215 [uid] => 1 [filename] => dicyclomine_s.jpg [filepath] => sites/default/files/images/dicyclomine_s.jpg [filemime] => image/jpeg [filesize] => 59686 [status] => 1 [timestamp] => 1329495177 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 253 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
IPICLOMIN®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>IPICLOMIN®
) [#title] => [#description] => [#children] =>IPICLOMIN®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>IPICLOMIN®
[#printed] => 1 ) [#title] => [#description] => [#children] =>IPICLOMIN®
Injection 20mg/2ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 20mg/2ml
) [#title] => [#description] => [#children] =>Injection 20mg/2ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 20mg/2ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 20mg/2ml
Antispasmodic/Anticholinegic
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antispasmodic/Anticholinegic
) [#title] => [#description] => [#children] =>Antispasmodic/Anticholinegic
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antispasmodic/Anticholinegic
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antispasmodic/Anticholinegic
Gastrointestinal drugs
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Gastrointestinal drugs
) [#title] => [#description] => [#children] =>Gastrointestinal drugs
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Gastrointestinal drugs
[#printed] => 1 ) [#title] => [#description] => [#children] =>Gastrointestinal drugs
Category B
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category B
) [#title] => [#description] => [#children] =>Category B
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category B
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category B
Dicyclomine relieves smooth muscle spasm of the gastrointestinal tract. Animal studies indicate that this action is achieved via a dual mechanism: (1) a specific anticholinergic effect (antimuscarinic) at the acetylcholine-receptor sites with approximately 1/8 the milligram potency of atropine (in vitro, guinea pig ileum); and (2) a direct effect upon smooth muscle (musculotropic) as evidenced by Dicyclomine’s antagonism of bradykinin- and histamine-induced spasms of the isolated guinea pig ileum. Atropine did not affect responses to these two agonists. In vivo studies in cats and dogs showed Dicyclomine to be equally potent against acetylcholine (ACh)- or barium chloride (BaCl2)-induced intestinal spasm while atropine was at least 200 times more potent against effects of ACh than BaCl2. Tests for mydriatic effects in mice showed that Dicyclomine was approximately 1/500 as potent as atropine; antisialagogue tests in rabbits showed Dicyclomine to be 1/300 as potent as atropine.
Dicyclomine can inhibit the secretion of saliva and sweat, decrease gastrointestinal secretions and motility, cause drowsiness, dilate the pupils, increase heart rate, and depress motor function.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
) [#title] => [#description] => [#children] =>Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 20mg/2ml: Box of 10 ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 20mg/2ml: Box of 10 ampoules
) [#title] => [#description] => [#children] =>• Injection 20mg/2ml: Box of 10 ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 20mg/2ml: Box of 10 ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 20mg/2ml: Box of 10 ampoules
IPICLOMIN®
Injection 20mg/2ml
Antispasmodic/Anticholinegic
Gastrointestinal drugs
Category B
Dicyclomine relieves smooth muscle spasm of the gastrointestinal tract. Animal studies indicate that this action is achieved via a dual mechanism: (1) a specific anticholinergic effect (antimuscarinic) at the acetylcholine-receptor sites with approximately 1/8 the milligram potency of atropine (in vitro, guinea pig ileum); and (2) a direct effect upon smooth muscle (musculotropic) as evidenced by Dicyclomine’s antagonism of bradykinin- and histamine-induced spasms of the isolated guinea pig ileum. Atropine did not affect responses to these two agonists. In vivo studies in cats and dogs showed Dicyclomine to be equally potent against acetylcholine (ACh)- or barium chloride (BaCl2)-induced intestinal spasm while atropine was at least 200 times more potent against effects of ACh than BaCl2. Tests for mydriatic effects in mice showed that Dicyclomine was approximately 1/500 as potent as atropine; antisialagogue tests in rabbits showed Dicyclomine to be 1/300 as potent as atropine.
Dicyclomine can inhibit the secretion of saliva and sweat, decrease gastrointestinal secretions and motility, cause drowsiness, dilate the pupils, increase heart rate, and depress motor function.
Absorption and Distribution
In man, dicyclomine is rapidly absorbed after oral administration, reaching peak values within 60 to 90 minutes. Mean volume of distribution for a 20 mg oral dose is approximately 3.65 L/kg suggesting extensive distribution in tissues.
Elimination
The metabolism of dicyclomine was not studied. The principal route of excretion is via the urine (79.5% of the dose). Excretion also occurs in the feces, but to a lesser extent (8.4%). Mean half-life of plasma elimination in one study was determined to be approximately 1.8 hours when plasma concentrations were measured for 9 hours after a single dose. In subsequent studies, plasma concentrations were followed for up to 24 hours after a single dose, showing a secondary phase of elimination with a somewhat longer half-life.
Dicyclomine hydrochloride oral solution is indicated for the treatment of functional bowel/irritable bowel syndrome.
• Obstructive uropathy
• Obstructive disease of the gastrointestinal tract
• Severe ulcerative colitis
• Reflux esophagitis
• Unstable cardiovascular status in acute hemorrhage
• Glaucoma
• Myasthenia gravis
• Evidence of prior hypersensitivity to Dicyclomine hydrochloride or other ingredients in this formulation
• Infants less than 6 months of age
• Nursing Mothers
Use with caution in patients with:
• Autonomic neuropathy
• Hepatic or renal disease
• Ulcerative colitis-large doses may suppress intestinal motility to the point of producing a paralytic ileus and the use of this drug may precipitate or aggravate the serious complication of toxic megacolon
• Hyperthyroidism
• Hypertension
• Coronary heart disease
• Congestive heart failure
• Cardiac tachyarrhythmia
• Hiatal hernia
• Known or suspected prostatic hypertrophy.
Investigate any tachycardia before administration of Dicyclomine hydrochloride, since it may increase the heart rate.
With overdosage, a curare-like action may occur (i.e., neuromuscular blockade leading to muscular weakness and possible paralysis).
The following agents may increase certain actions or side effects of anticholinergic drugs: amantadine, antiarrhythmic agents of Class I (e.g., quinidine), antihistamines, antipsychotic agents (e.g., phenothiazines), benzodiazepines, MAO inhibitors, narcotic analgesics (e.g., meperidine), nitrates and nitrites, sympathomimetic agents, tricyclic antidepressants, and other drugs having anticholinergic activity.
Anticholinergics antagonize the effects of antiglaucoma agents. Anticholinergic drugs in the presence of increased intraocular pressure may be hazardous when taken concurrently with agents such as corticosteroids.
Anticholinergic agents may affect gastrointestinal absorption of various drugs, such as slowly dissolving dosage forms of digoxin; increased serum digoxin concentrations may result. Anticholinergic drugs may antagonize the effects of drugs that alter gastrointestinal motility, such as metoclopramide. Because antacids may interfere with the absorption of anticholinergic agents, simultaneous use of these drugs should be avoided.
The inhibiting effects of anticholinergic drugs on gastric hydrochloric acid secretion are antagonized by agents used to treat achlorhydria and those used to test gastric secretion.
Gastrointestinal: dry mouth, nausea, vomiting, constipation, bloated feeling, abdominal pain, taste loss, anorexia.
Central Nervous System: dizziness, lightheadedness, tingling, headache, drowsiness, weakness, nervousness, numbness, mental confusion and/or excitement (especially in elderly persons), dyskinesia, lethargy, syncope, speech disturbance, insomnia.
Ophthalmologic: blurred vision, diplopia, mydriasis, cycloplegia, increased ocular tension
Dermatologic/Allergic: rash, urticaria, itching, and other dermal manifestations; severe allergic reaction or drug idiosyncrasies including anaphylaxis.
Genitourinary: urinary hesitancy, urinary retention
Cardiovascular: tachycardia. palpitations
Respiratory: Dyspnea, apnea, asphyxia
Other: decreased sweating, nasal stuffiness or congestion, sneezing, throat congestion, impotence, suppression of lactation
• Store below 30 C°
• Protect from light and freezing
• Injection 20mg/2ml: Box of 10 ampoules