Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Amikacin
Pharmacology
Intramuscular Administration
Amikacin is rapidly absorbed after intramuscular administration. In normal adult volunteers, average peak serum concentrations of about 12, 16 and 21 mcg/mL are obtained 1 hour after intramuscular administration of 250 mg (3.7 mg/kg), 375 mg (5 mg/kg), 500 mg (7.5 mg/kg), single doses, respectively. At 10 hours, serum levels are about 0.3 mcg/mL, 1.2 mcg/mL and 2.1 mcg/mL, respectively.
Tolerance studies in normal volunteers reveal that Amikacin is well tolerated locally following repeated intramuscular dosing, and when given at maximally recommended doses, no ototoxicity or nephrotoxicity has been reported. There is no evidence of drug accumulation with repeated dosing for 10 days when administered according to recommended doses.
With normal renal function, about 91.9% of an intramuscular dose is excreted unchanged in the urine in the first 8 hours and 98.2% within 24 hours. Mean urine concentrations for 6 hours are 563 mcg/mL following a 250 mg dose, 697 mcg/mL following a 375 mg dose and 832 mcg/mL following a 500 mg dose.
Preliminary intramuscular studies in newborns of different weights (less than 1.5 kg, 1.5 to 2 kg, over 2 kg) at a dose of 7.5 mg/kg revealed that, like other aminoglycosides, serum half-life values were correlated inversely with post-natal age and renal clearances of Amikacin. The volume of distribution indicates that Amikacin, like other aminoglycosides, remains primarily in the extra-cellular fluid space of neonates. Repeated dosing every 12 hours in all the above groups did not demonstrate accumulation after 5 days.
Intravenous Administration
Single doses of 500 mg (7.5 mg/kg) administered to normal adults as an infusion over a period of 30 minutes produced a mean peak serum concentration of 38 mcg/mL at the end of the infusion and levels of 24 mcg/mL, 18 mcg/mL and 0.75 mcg/mL at 30 minutes, 1 hour and 10 hours post-infusion, respectively. Eighty-four percent of the administered dose was excreted in the urine in 9 hours and about 94% within 24 hours.
Repeat infusions of 7.5 mg/kg every 12 hours in normal adults were well tolerated and caused no drug accumulation.
Pharmacokinetics:
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Indications:
Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Contraindications:
A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
Precautions:
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Drug Interactions:
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
Side Effects:
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
Storage:
• Store below 30 C°
• Protect from light and freezing
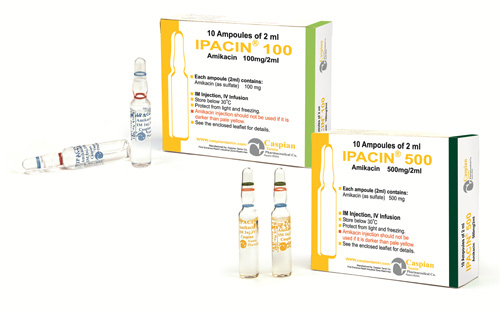
Packing:
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
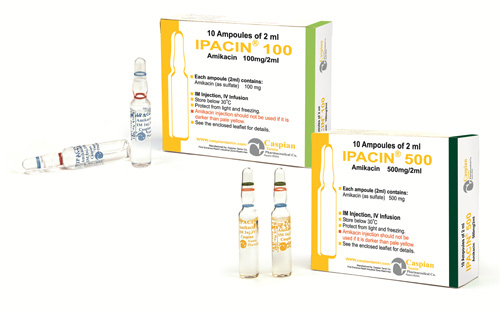
IPACIN®
Injection 100mg/2ml- Injection 500mg/2ml
Aminoglycosides
Antibiotic
Category D
Intramuscular Administration
Amikacin is rapidly absorbed after intramuscular administration. In normal adult volunteers, average peak serum concentrations of about 12, 16 and 21 mcg/mL are obtained 1 hour after intramuscular administration of 250 mg (3.7 mg/kg), 375 mg (5 mg/kg), 500 mg (7.5 mg/kg), single doses, respectively. At 10 hours, serum levels are about 0.3 mcg/mL, 1.2 mcg/mL and 2.1 mcg/mL, respectively.
Tolerance studies in normal volunteers reveal that Amikacin is well tolerated locally following repeated intramuscular dosing, and when given at maximally recommended doses, no ototoxicity or nephrotoxicity has been reported. There is no evidence of drug accumulation with repeated dosing for 10 days when administered according to recommended doses.
With normal renal function, about 91.9% of an intramuscular dose is excreted unchanged in the urine in the first 8 hours and 98.2% within 24 hours. Mean urine concentrations for 6 hours are 563 mcg/mL following a 250 mg dose, 697 mcg/mL following a 375 mg dose and 832 mcg/mL following a 500 mg dose.
Preliminary intramuscular studies in newborns of different weights (less than 1.5 kg, 1.5 to 2 kg, over 2 kg) at a dose of 7.5 mg/kg revealed that, like other aminoglycosides, serum half-life values were correlated inversely with post-natal age and renal clearances of Amikacin. The volume of distribution indicates that Amikacin, like other aminoglycosides, remains primarily in the extra-cellular fluid space of neonates. Repeated dosing every 12 hours in all the above groups did not demonstrate accumulation after 5 days.
Intravenous Administration
Single doses of 500 mg (7.5 mg/kg) administered to normal adults as an infusion over a period of 30 minutes produced a mean peak serum concentration of 38 mcg/mL at the end of the infusion and levels of 24 mcg/mL, 18 mcg/mL and 0.75 mcg/mL at 30 minutes, 1 hour and 10 hours post-infusion, respectively. Eighty-four percent of the administered dose was excreted in the urine in 9 hours and about 94% within 24 hours.
Repeat infusions of 7.5 mg/kg every 12 hours in normal adults were well tolerated and caused no drug accumulation.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
• Store below 30 C°
• Protect from light and freezing
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPACIN®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => IPACIN®
[format] => 1
[safe] => IPACIN®
[view] =>IPACIN®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class. [format] => 1 [safe] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
[view] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 100mg/2ml- Injection 500mg/2ml [format] => 1 [safe] =>Injection 100mg/2ml- Injection 500mg/2ml
[view] =>Injection 100mg/2ml- Injection 500mg/2ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => These drugs known to have major interactions with Amikacin: botulinumtoxinA AccessPak for HIV PEP Basic (emtricitabine / tenofovir) AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir) AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir) adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin, magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate, tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid, polymyxin b, succinylcholine [format] => 1 [safe] =>These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
[view] =>Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 100mg/2ml: Box of 10Ampoules • Injection 500mg/2ml: Box of 10Ampoules [format] => 1 [safe] =>• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Aminoglycosides
[view] =>Aminoglycosides
) ) [field_precautions] => Array ( [0] => Array ( [value] => Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation. Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations. Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment. If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped. Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important. Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction. In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase). Cross-allergenicity among aminoglycosides has been demonstrated. As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted. Aminoglycosides should not be given concurrently with potent diuretics [format] => 1 [safe] =>Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Category D
[view] =>Category D
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] =>General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
[format] => 1 [safe] =>General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Antibiotic
[view] =>Antibiotic
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [10] => stdClass Object ( [tid] => 10 [vid] => 1 [name] => Antibacterials [description] => [weight] => 8 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 830 [uid] => 1 [filename] => injection-amikacin_10050.jpg [filepath] => sites/default/files/images/injection-amikacin_10050.jpg [filemime] => image/jpeg [filesize] => 45237 [status] => 1 [timestamp] => 1375599312 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 280 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>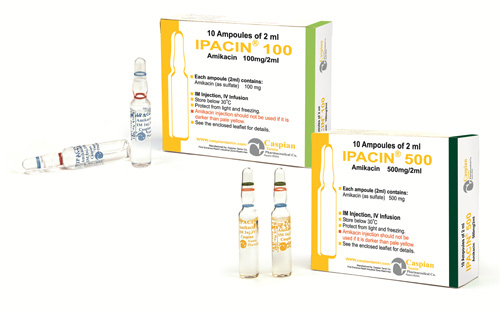 )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] => 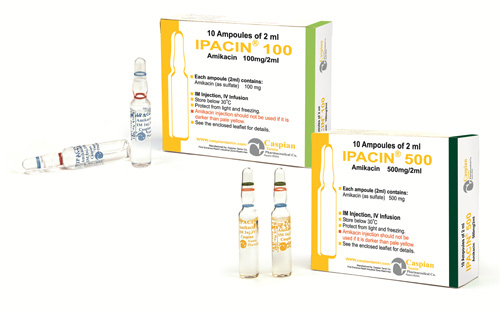 [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] => 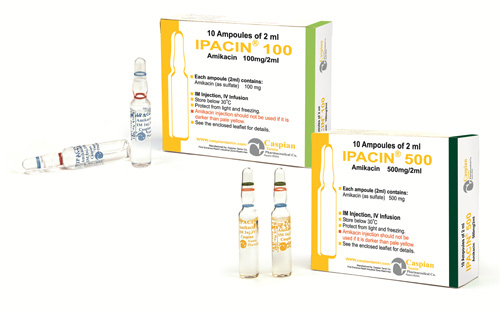 [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 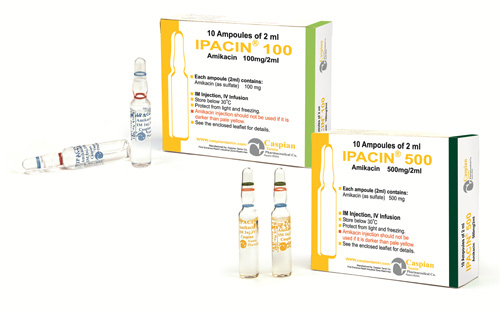
IPACIN®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>IPACIN®
) [#title] => [#description] => [#children] =>IPACIN®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>IPACIN®
[#printed] => 1 ) [#title] => [#description] => [#children] =>IPACIN®
Injection 100mg/2ml- Injection 500mg/2ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 100mg/2ml- Injection 500mg/2ml
) [#title] => [#description] => [#children] =>Injection 100mg/2ml- Injection 500mg/2ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 100mg/2ml- Injection 500mg/2ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 100mg/2ml- Injection 500mg/2ml
Aminoglycosides
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Aminoglycosides
) [#title] => [#description] => [#children] =>Aminoglycosides
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Aminoglycosides
[#printed] => 1 ) [#title] => [#description] => [#children] =>Aminoglycosides
Antibiotic
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antibiotic
) [#title] => [#description] => [#children] =>Antibiotic
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antibiotic
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antibiotic
Category D
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category D
) [#title] => [#description] => [#children] =>Category D
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category D
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category D
Intramuscular Administration
Amikacin is rapidly absorbed after intramuscular administration. In normal adult volunteers, average peak serum concentrations of about 12, 16 and 21 mcg/mL are obtained 1 hour after intramuscular administration of 250 mg (3.7 mg/kg), 375 mg (5 mg/kg), 500 mg (7.5 mg/kg), single doses, respectively. At 10 hours, serum levels are about 0.3 mcg/mL, 1.2 mcg/mL and 2.1 mcg/mL, respectively.
Tolerance studies in normal volunteers reveal that Amikacin is well tolerated locally following repeated intramuscular dosing, and when given at maximally recommended doses, no ototoxicity or nephrotoxicity has been reported. There is no evidence of drug accumulation with repeated dosing for 10 days when administered according to recommended doses.
With normal renal function, about 91.9% of an intramuscular dose is excreted unchanged in the urine in the first 8 hours and 98.2% within 24 hours. Mean urine concentrations for 6 hours are 563 mcg/mL following a 250 mg dose, 697 mcg/mL following a 375 mg dose and 832 mcg/mL following a 500 mg dose.
Preliminary intramuscular studies in newborns of different weights (less than 1.5 kg, 1.5 to 2 kg, over 2 kg) at a dose of 7.5 mg/kg revealed that, like other aminoglycosides, serum half-life values were correlated inversely with post-natal age and renal clearances of Amikacin. The volume of distribution indicates that Amikacin, like other aminoglycosides, remains primarily in the extra-cellular fluid space of neonates. Repeated dosing every 12 hours in all the above groups did not demonstrate accumulation after 5 days.
Intravenous Administration
Single doses of 500 mg (7.5 mg/kg) administered to normal adults as an infusion over a period of 30 minutes produced a mean peak serum concentration of 38 mcg/mL at the end of the infusion and levels of 24 mcg/mL, 18 mcg/mL and 0.75 mcg/mL at 30 minutes, 1 hour and 10 hours post-infusion, respectively. Eighty-four percent of the administered dose was excreted in the urine in 9 hours and about 94% within 24 hours.
Repeat infusions of 7.5 mg/kg every 12 hours in normal adults were well tolerated and caused no drug accumulation.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function. Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under. Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids. Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively. [format] => 1 [safe] =>Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
) [#title] => [#description] => [#children] =>Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
) [#title] => [#description] => [#children] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
[#printed] => 1 ) [#title] => [#description] => [#children] =>A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
[format] => 1 [safe] =>General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules
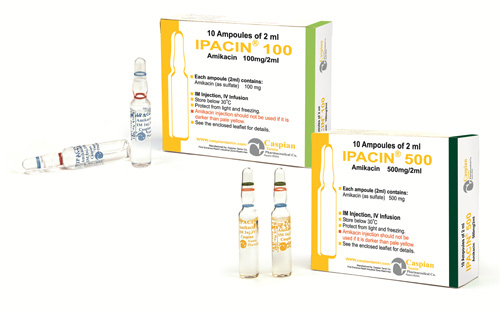
IPACIN®
Injection 100mg/2ml- Injection 500mg/2ml
Aminoglycosides
Antibiotic
Category D
Intramuscular Administration
Amikacin is rapidly absorbed after intramuscular administration. In normal adult volunteers, average peak serum concentrations of about 12, 16 and 21 mcg/mL are obtained 1 hour after intramuscular administration of 250 mg (3.7 mg/kg), 375 mg (5 mg/kg), 500 mg (7.5 mg/kg), single doses, respectively. At 10 hours, serum levels are about 0.3 mcg/mL, 1.2 mcg/mL and 2.1 mcg/mL, respectively.
Tolerance studies in normal volunteers reveal that Amikacin is well tolerated locally following repeated intramuscular dosing, and when given at maximally recommended doses, no ototoxicity or nephrotoxicity has been reported. There is no evidence of drug accumulation with repeated dosing for 10 days when administered according to recommended doses.
With normal renal function, about 91.9% of an intramuscular dose is excreted unchanged in the urine in the first 8 hours and 98.2% within 24 hours. Mean urine concentrations for 6 hours are 563 mcg/mL following a 250 mg dose, 697 mcg/mL following a 375 mg dose and 832 mcg/mL following a 500 mg dose.
Preliminary intramuscular studies in newborns of different weights (less than 1.5 kg, 1.5 to 2 kg, over 2 kg) at a dose of 7.5 mg/kg revealed that, like other aminoglycosides, serum half-life values were correlated inversely with post-natal age and renal clearances of Amikacin. The volume of distribution indicates that Amikacin, like other aminoglycosides, remains primarily in the extra-cellular fluid space of neonates. Repeated dosing every 12 hours in all the above groups did not demonstrate accumulation after 5 days.
Intravenous Administration
Single doses of 500 mg (7.5 mg/kg) administered to normal adults as an infusion over a period of 30 minutes produced a mean peak serum concentration of 38 mcg/mL at the end of the infusion and levels of 24 mcg/mL, 18 mcg/mL and 0.75 mcg/mL at 30 minutes, 1 hour and 10 hours post-infusion, respectively. Eighty-four percent of the administered dose was excreted in the urine in 9 hours and about 94% within 24 hours.
Repeat infusions of 7.5 mg/kg every 12 hours in normal adults were well tolerated and caused no drug accumulation.
Pharmacokinetic studies in normal adult subjects reveal the mean serum half-life to be slightly over 2 hours with a mean total apparent volume of distribution of 24 liters (28% of the body weight). By the ultrafiltration technique, reports of serum protein binding range from 0 to 11%. The mean serum clearance rate is about 100 mL/min and the renal clearance rate is 94 mL/min in subjects with normal renal function.
Amikacin is excreted primarily by glomerular filtration. Patients with impaired renal function or diminished glomerular filtration pressure excrete the drug much more slowly (effectively prolonging the serum half-life). Therefore, renal function should be monitored carefully and dosage adjusted accordingly (see suggested dosage schedule under.
Following administration at the recommended dose, therapeutic levels are found in bone, heart, gallbladder, and lung tissue in addition to significant concentrations in urine, bile, sputum, bronchial secretions, interstitial, pleural, and synovial fluids.
Spinal fluid levels in normal infants are approximately 10 to 20% of the serum concentrations and may reach 50% when the meninges are inflamed. Amikacin has been demonstrated to cross the placental barrier and yield significant concentrations in amniotic fluid. The peak fetal serum concentration is about 16% of the peak maternal serum concentration and maternal and fetal serum half-life values are about 2 and 3.7 hours, respectively.
Amikacin sulfate is indicated in the short-term treatment of serious infections due to susceptible strains of Gram-negative bacteria, including Pseudomonas species, Escherichia coli, species of indole-positive and indole-negative Proteus, Providencia species, Klebsiella-Enterobacter-Serratia species and Acinetobacter (Mima-Herellea) species.
Clinical studies have shown Amikacin sulfate to be effective in bacterial septicemia (including neonatal sepsis); in serious infections of the respiratory tract, bones and joints, central nervous system (including meningitis) and skin and soft tissue; intra-abdominal infections (including peritonitis); and in burns and postoperative infections (including post-vascular surgery). Clinical studies have shown Amikacin also to be effective in serious complicated and recurrent urinary tract infections due to these organisms. Aminoglycosides, including Amikacin sulfate are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity.
Bacteriologic studies should be performed to identify causative organisms and their susceptibilities to Amikacin. Amikacin may be considered as initial therapy in suspected gram-negative infections, and therapy may be instituted before obtaining the results of susceptibility testing. Clinical trials demonstrated that Amikacin was effective in infections caused by gentamicin- and/or tobramycin-resistant strains of gram-negative organisms, particularly Proteus rettgeri, Providencia stuartii, Serratia marcescens and Pseudomonas aeruginosa. The decision to continue therapy with the drug should be based on results of the susceptibility tests, the severity of the infection, the response of the patient and the important additional considerations .
Amikacin has also been shown to be effective in staphylococcal infections and may be considered as initial therapy under certain conditions in the treatment of known or suspected staphylococcal disease such as, severe infections where the causative organism may be either a gram-negative bacterium or a staphylococcus, infections due to susceptible strains of staphylococci in patients allergic to other antibiotics, and in mixed staphylococcal/gram-negative infections.
In certain severe infections such as neonatal sepsis, concomitant therapy with a penicillin-type drug may be indicated because of the possibility of infections due to gram-positive organisms such as streptococci or pneumococci.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Amikacin sulfate and other antibacterial drugs, Amikacin sulfate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
A history of hypersensitivity to Amikacin is a contraindication for its use. A history of hypersensitivity or serious toxic reactions to aminoglycosides may contraindicate the use of any other aminoglycoside because of the known cross-sensitivities of patients to drugs in this class.
Prescribing Amikacin sulfate injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Aminoglycosides are quickly and almost totally absorbed when they are applied topically, except to the urinary bladder, in association with surgical procedures. Irreversible deafness, renal failure and death due to neuromuscular blockade have been reported following irrigation of both small and large surgical fields with an aminoglycoside preparation.
Amikacin sulfate injection is potentially nephrotoxic, ototoxic and neurotoxic. The concurrent or serial use of other ototoxic or nephrotoxic agents should be avoided either systemically or topically because of the potential for additive effects. Increased nephrotoxicity has been reported following concomitant parenteral administration of aminoglycosides, antibiotics and cephalosporins. Concomitant cephalosporins may spuriously elevate creatinine determinations.
Since Amikacin is present in high concentrations in the renal excretory system, patients should be well-hydrated to minimize chemical irritation of the renal tubules. Kidney function should be assessed by the usual methods prior to starting therapy and daily during the course of treatment.
If signs of renal irritation appear (casts, white or red cells or albumin), hydration should be increased. A reduction in dosage may be desirable if other evidence of renal dysfunction occurs such as decreased creatinine clearance; decreased urine specific gravity; increased BUN, creatinine or oliguria. If azotemia increases or if a progressive decrease in urinary output occurs, treatment should be stopped.
Elderly patients may have reduced renal function which may not be evident in routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with aminoglycosides is particularly important.
Aminoglycosides should be used with caution in patients with muscular disorders such as myasthenia gravis or parkinsonism since these drugs may aggravate muscle weakness because of their potential curare-like effect on the neuromuscular junction.
In vitro mixing of aminoglycosides with beta-lactam antibiotics (penicillin or cephalosporins) may result in a significant mutual inactivation. A reduction in serum half-life or serum level may occur when an aminoglycoside or penicillin-type drug is administered by separate routes. Inactivation of the aminoglycoside is clinically significant only in patients with severely impaired renal function. Inactivation may continue in specimens of body fluids collected for assay, resulting in inaccurate aminoglycoside readings. Such specimens should be properly handled (assayed promptly, frozen or treated with betalactamase).
Cross-allergenicity among aminoglycosides has been demonstrated.
As with other antibiotics, the use of Amikacin may result in overgrowth of non-susceptible organisms. If this occurs, appropriate therapy should be instituted.
Aminoglycosides should not be given concurrently with potent diuretics
These drugs known to have major interactions with Amikacin:
botulinumtoxinA
AccessPak for HIV PEP Basic (emtricitabine / tenofovir)
AccessPak for HIV PEP Expanded with Kaletra (emtricitabine / lopinavir / ritonavir / tenofovir)
AccessPak for HIV PEP Expanded with Viracept (emtricitabine / nelfinavir / tenofovir)
adefovir, cidofovir, tenofovir, streptomycin, tobramycin capreomycin, Carimune
pipecuronium, doxacurium, vecuronium, mivacurium, rocuronium, pancuronium
cisatracurium, rapacuronium, gentamicin, kanamycin, neomycin, netilmicin,
magnesium sulfate, metocurine, sirolimus, tacrolimus, bumetanide, gallium nitrate,
tubocurarine, colistimethate, deferasirox, torsemide, furosemide, ethacrynic acid,
polymyxin b, succinylcholine
General
All aminoglycosides have the potential to cause auditory, vestibular, and renal toxicity and neuromuscular blockade. Such side effects occurred more often in patients with current or past history of renal impairment, of treatment with other ototoxic or nephrotoxic agents, and in patients treated for longer periods and/or with higher doses than recommended.
Renal
Such renal function changes were usually reversible when the drug was discontinued.
Predisposing factors have included advanced age, preexisting renal insufficiency, dehydration, and concomitant use of other potentially nephrotoxic drugs. One study has shown that hyperbilirubinemia in patients with biliary obstruction may also be a predisposing factor to aminoglycoside nephrotoxicity.
In one prospective, nonrandomized study, patients developed nephrotoxicity in 25% of amikacin courses.
Frequency not reported: Nephrotoxicity, elevated serum creatinine, albuminuria, presence of red and white cells, casts, azotemia, oliguria
Nervous system
Ototoxicity may be irreversible and usually includes loss of auditory function secondary to cochlear hair cell damage. Damage may also be vestibular.
High frequency deafness usually occurs before hearing loss can be detected. Hearing loss may be permanent.
Rare neurologic side effects have included neuromuscular blockade, particularly in patients who are predisposed, including patients with myasthenia gravis, hypocalcemia, and patients on concomitant neuromuscular blocking agents.
Rare (less than 0.1%): Headache, paresthesia, tremor
Frequency not reported: Neurotoxicity, ototoxicity (including vestibular and permanent bilateral auditory ototoxicity), neuromuscular blockade, toxic effects on the eighth cranial nerve, hearing loss, loss of balance, cochlear damage, high frequency deafness, total or partial irreversible bilateral deafness, acute muscular paralysis due to neuromuscular blockade, numbness, skin tingling, muscle twitching, convulsions, dizziness, vertigo, tinnitus, roaring in the ears
Respiratory
Frequency not reported: Respiratory paralysis/apnea due to neuromuscular blockade
Musculoskeletal
Rare (less than 0.1%): Arthralgia
Gastrointestinal
Rare (less than 0.1%): Nausea, vomiting
Hematologic
Rare (less than 0.1%): Anemia, eosinophilia
Cardiovascular
Rare (less than 0.1%): Hypotension
Frequency not reported: Hypersensitivity myocarditis
Dermatologic
Rare (less than 0.1%): Skin rash, pruritus, exfoliative dermatitis
Other
Rare (less than 0.1%): Fever, drug fever
Hypersensitivity
Rare (less than 0.1%): Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome (at least 1 case)
Hepatic
Frequency not reported: Elevations in liver function tests (clinical significance unknown)
• Store below 30 C°
• Protect from light and freezing
• Injection 100mg/2ml: Box of 10Ampoules
• Injection 500mg/2ml: Box of 10Ampoules